How closely related are coronavirus and dementia? Can the new virus cause death in patients who are diagnosed with dementia and any other related states, like Alzheimer’s disease and vascular dementia?
Country lockdowns, new infections, thousands of fatalities, are some of the negative effects of the newly discovered coronavirus disease or COVID-19.
Information from China where the disease started states that some people are at higher risk of getting very ill from the disease.
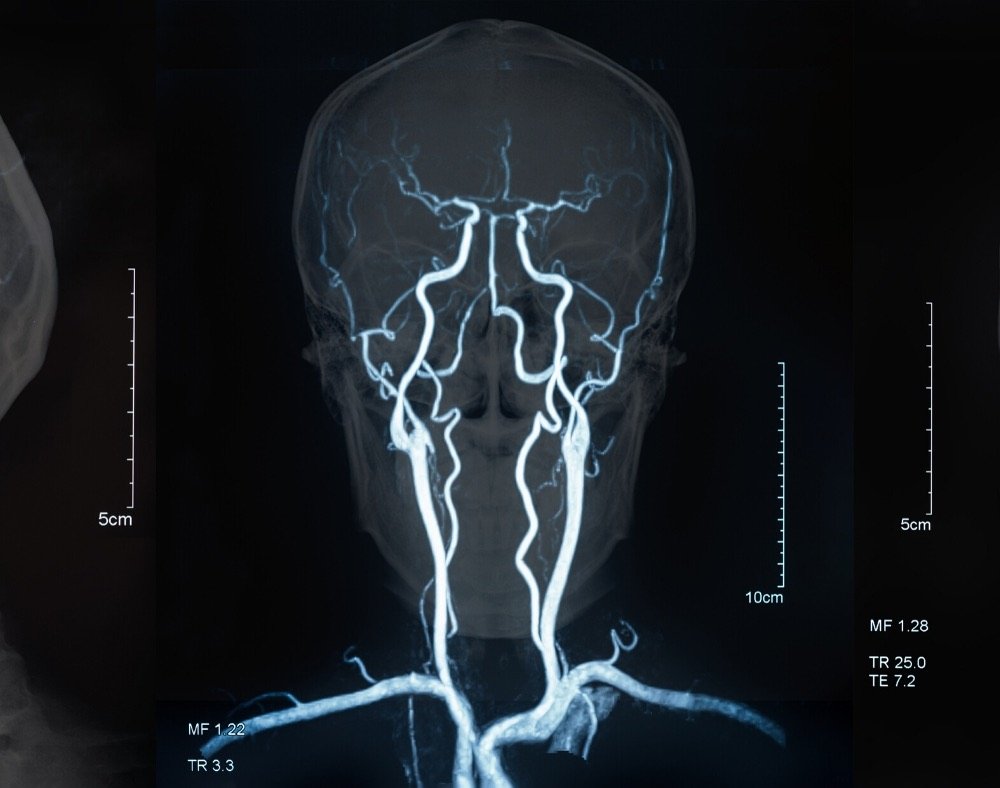
These include older people and individuals who have chronic medical conditions like lung disease, heart disease, and diabetes.
Statistically, a high percentage of persons with dementia are seniors.
This automatically puts them at a higher risk of contracting coronavirus disease in regions where the virus is spreading like wildfire.
Coronavirus and Dementia Risk
It must be tough for one person to suffer from both coronavirus and dementia.
For this reason, it is best to keep individuals with dementia safe from the virus.
Before we look into the steps to prevent people from dementia from contracting the virus, here is an overview of the coronavirus illness.
What is COVID-19?

It is an infectious disease that the newly discovered coronavirus causes. The disease and the virus were unknown before an outbreak began in December 2019 in Wuhan, China.
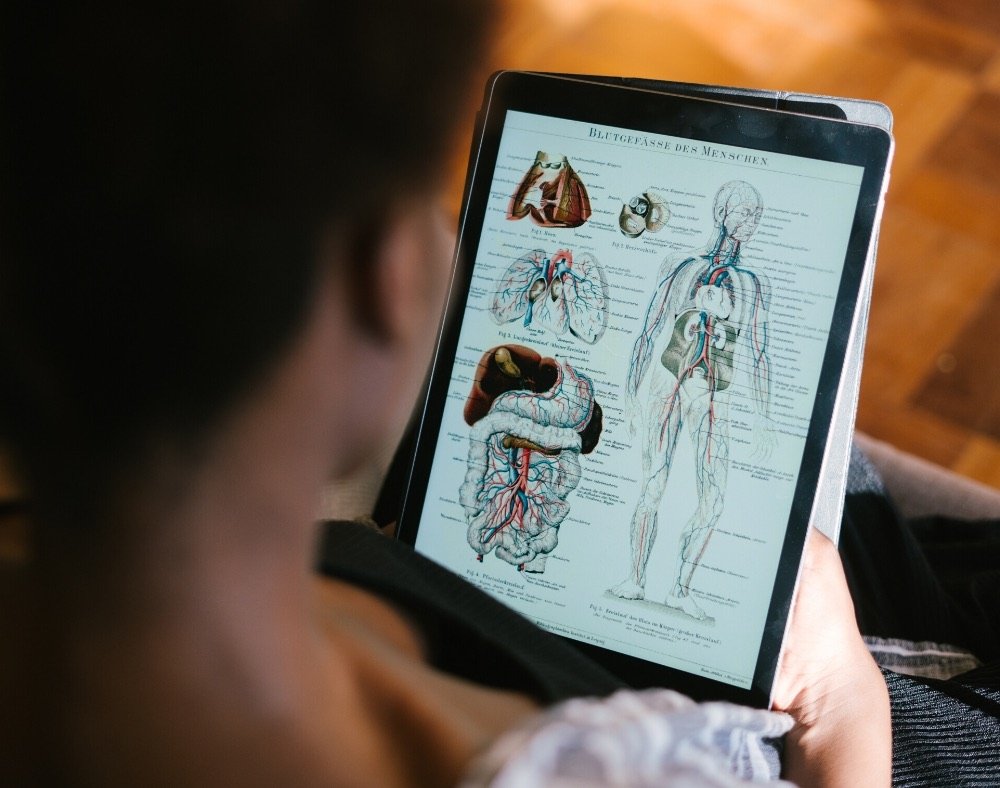
WHO (World Health Organization) describes coronavirus as a huge family of viruses that may cause illness in both humans and animals.
Symptoms of Coronavirus Disease

You can find some of the potential warning signs of COVID-19 below. Note that the list is not inclusive.
- Dry cough
- Fever
- Shortness of breath
- Tiredness
- Persistent pressure or pain in the chest
- Sore throat
- Nasal congestion
- Diarrhea
Anyone who develops the symptoms must immediately get medical attention.
Worth noting is that some people will become infected without feeling unwell or developing any symptoms.
About 80% of the people with the disease recover without needing special treatment.
Protect Persons With Dementia From Coronavirus
When it comes to protecting persons with dementia from the coronavirus disease, there are a few steps caregivers and the weak individuals can take such as:
Stick to Essential Hygienic Practices

It is very easy for persons with dementia to forget about daily hygienic practices which might increase the risk of getting the disease from coronavirus and dementia.
Caregivers may need to step in to offer reminders or help them execute duties like washing hands with warm water and soap.
Demonstrate or offer a hand where necessary so that the ill person knows how to wash their hands well for about 20 seconds. If a person cannot always wash their hands, they can use an alcohol-based sanitizer with a minimum of 70% alcohol.
While caring for a person with dementia, it also helps to keep an eye on them so that they do not touch their mouth, eyes, or nose.
Additionally, it is also vital to disinfect and clean all the surfaces that ill individuals touch daily.
This can include things such as sinks, faucets, keyboards, handles, light switches, tables, countertops, desks, phones, and toilets.
Understand How the Virus Spreads

Currently, both coronavirus and dementia have no cures or vaccines. According to the CDC (Centre or Disease Control and Prevention), one of the best ways to prevent a person from getting the virus is to avoid its exposure.
Scientists believe that it primarily spreads from one person to another through respiratory droplets that infected person produces when they cough or sneeze.
When these droplets land into your nose or mouth, you inhale them into your lungs and you end up with coronavirus disease.
It is, therefore, imperative to put persons with dementia at a safe distance from other people especially if the community around them is affected by the viral illness.
It is also advisable for persons with dementia to stock up on supplies, including groceries and household items that will enable them to stay at home for long periods until health officials confirm that it is safe to go about regular businesses.
Shopping online and mail order medications can come in handy during tough times.
Limit Number of Trips

The burden of coronavirus and dementia on one person may be too much to handle. For this reason, it is important to limit the movements of the person with dementia so that their chances of contracting the virus are significantly reduced.
It would be best if they stay at home or in their facility without leaving until the situation is contained. Persons with dementia should hold off on taking any trips by road, air or sea.
Think and Plan Ahead
Based on how infections seem to skyrocket within no time, caregivers also need to think of alternative care plans should anything change in the future because of the COVID-19.
Think of possibilities like the primary caregiver getting infected. They will not be in a position to execute their caring duties and the person with dementia cannot be abandoned.
The individual with dementia may also not be able to access services like respite care or adult day care services if the region they are in is experiencing a lockdown and people cannot move about freely.
It is vital to come up with alternative plans beforehand; things do not go south if the virus causes unimaginable changes.
Closing Thoughts
It is scary to think about the effects of coronavirus and dementia on a person.
However, taking the necessary precautions may keep suffering people safe from the recently discovered disease.
Remember to keep medical contacts close by so that you can contact medics if you feel like you have symptoms of the disease.
It is also important to stay up to date about the coronavirus disease from reliable sources.
Scientists continue monitoring and responding to the pandemic because they still do not fully understand the complete clinical picture of the disease.