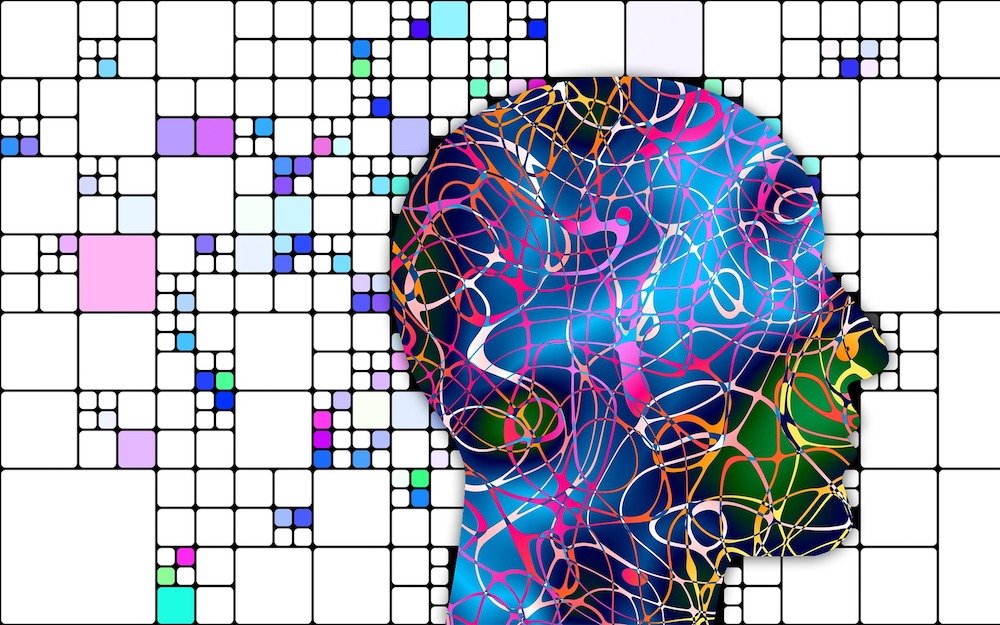
We studied and conducted a complete overview of self-explanatory mixed dementia.
People who have dementia may experience changes that represent TWO OR MORE types of dementia occurring simultaneously in the brain.
This disorder is quite complex.
There are several combinations possible which can be a mixture of one, two or even more of the types of dementia below:
- Vascular dementia
- Alzheimer’s disease
- Dementia with Lewy bodies
- Multi-infarct dementia
- Strategic infract dementia
- Subcortical vascular dementia
- Parkinson’s disease dementia
- Frontotemporal dementia
- Semantic dementia
- Alcohol-related dementia
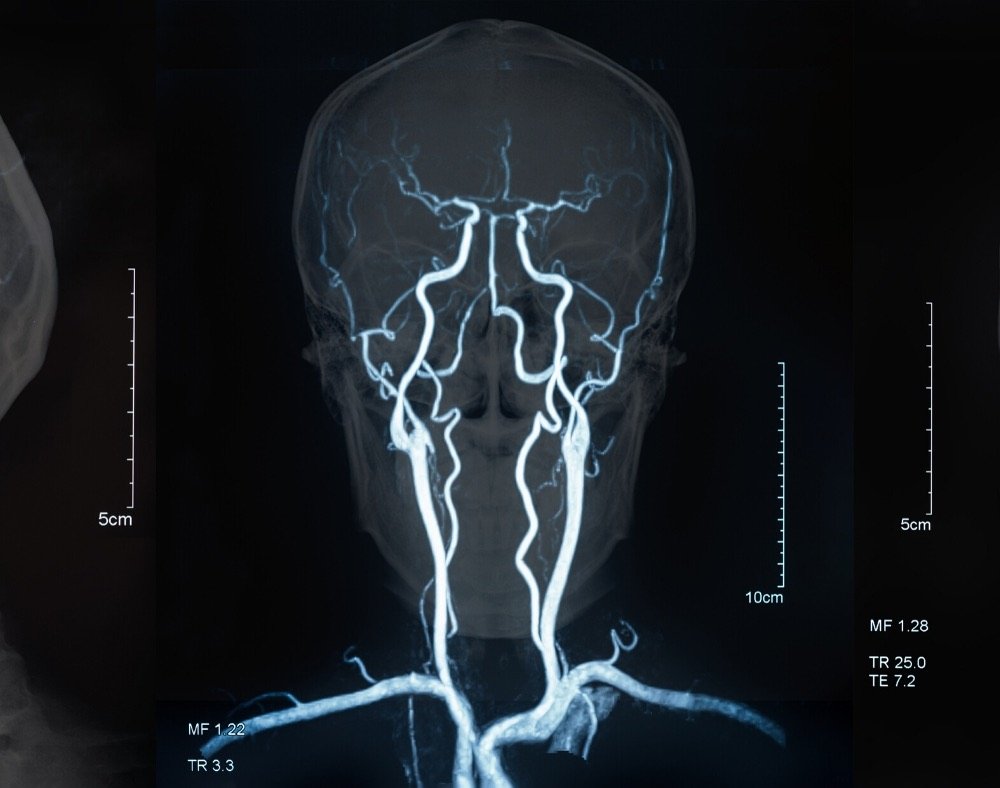
The most common cases are usually a combination between blood vessel abnormalities commonly linked with vascular dementia and protein deposits usually seen in Alzheimer’s disease.
It is believed that about 10% of people with dementia also have the illness.
Scientists, however, reveal that this number could be HIGHER.
The illness may occur in different stages. These are important when it comes to guiding caregivers and physicians on how to best take care of people with this kind of dementia.
Below are seven common stages of mixed dementia.
7 Stages Of Mixed Dementia
1. No impairment

This is where an individual can go about their business and life independently.
During this stage, there are no outward clear signs of the illness. At this stage, it is more or less if someone else suggests testing ourselves for (mixed) dementia or we read it in an article – like this one.
Since dementia starts developing years and years in advance, anyone at the age of around fifty should test themselves.
Sometimes even earlier.
2. Very Mild
The signs and symptoms at this stage also hardly manifest. Generally, there may appear normal forgetfulness signs that are associated with aging.
For instance, a person may struggle to remember the name of a loved one, but finally, figure it out after some time.
If these events start to repeat, become almost annoying, the individual should visit the doctor.
3. Mild

During this point, the symptoms remain barely noticeable. A person may go on their daily lives without too much interruption.
Some people may, however, showcase symptoms such as repetition, slight memory loss, loss of concentration and difficulties managing finances such as balancing checkbooks.
Again if the person is doing the same mistakes again and again or forgetting the name of the same person, seeing the doctor is almost crucial.
4. Moderate

It becomes clear at this stage that many people cannot complete routine tasks without some form of assistance.
This can be SIMPLE THINGS such as preparing meals, using the phone, changing television programs and completing laundry.
Some people also start to withdraw socially, experience incontinence and have trouble finding the right phrases or words.
5. Moderately Severe

During these final stages, people with this kind of dementia need help to go about their day to day lives.
Some symptoms may include an increase in memory loss, confusion regarding events, and current location.
Also, the need for a helping hand when picking appropriate clothing and tying shoelaces.
6. Severe

The disease becomes worse at this stage and individuals can no longer perform duties on their own.
They may need a helping hand with a majority of their day-to-day activities including when dressing, going to the toilet, eating, walking, and sleeping.
At this time, a caregiver is almost a necessity.
7. Very Severe

The final stage is associated with signs like LOSS of muscle control, hard times with language ability, no control over urination, and losing awareness of the surroundings.
With this type of dementia, hence the name, several different symptoms and signs may occur from several other different dementias.
Mixed Dementia Symptoms
Worth noting is that a diagnosis of mixed dementia is quite difficult.
Most people with the illness do not know that they have it because the many brain changes it involves are hard to detect.
Instead, persons are usually diagnosed with the kind of dementia that best suits the symptoms they have.
Many are the times when the disease is only seen during an autopsy rather than during life.
Depending on the dementia combination that a person has, the symptoms may vary widely.
Primarily, the symptoms are similar to those of a specific type of dementia or Alzheimer’s disease.
Some people’s symptoms may be a clear indication of the existence of multiple kinds of dementia. These may include:
Learning Difficulties
Trouble remembering newly acquired information is one of the earliest signs that people with dementia have.
You can teach a person something new today and if asked about it tomorrow, they may not know what you are talking about.
The reason for this is that dementia characteristically affects the section of the brain that is responsible for learning.
As a person grows older and the disease becomes worse, they may report more severe symptoms.
These can include disorientation, changes in behavior/mood, worsening confusion of places, time, and event, and becoming suspicious of friends, family members, or the caregivers who spend quality time with the individual with this type of dementia.
Loss of Memory

Everyone with dementia at one point experiences difficulties with memory. It usually starts off light something that does not bother many.
Trouble sets in when the loss of memory begins to interfere with a person’s ability to perform their normal daily tasks.
Signs of this may include the increasing need to rely on aids such as reminder notes or electronic devices to remember stuff.
Some people will even forget the most important dates of their lives like their birthdays, children’s/ partner’s birthdates, doctor’s appointments, and so on.
Many people with dementia also get into the habit of asking for the same details repeatedly.
Additionally, they may also lose things frequently and leave valuable items in unusual places.
Poor Judgement

People with mixed dementia may have a difficult time making the right call whenever necessary.
For instance, you may find that an individual does not have control over their money.
They may become over generous giving up huge chunks of money to telemarketers and other organizations.
Such people are usually vulnerable and they need a trustworthy person to guide them since they can easily fall into the hands of conmen.
As the disease, progresses, people with the illness may start to pay less attention to their bodies ignoring basic hygiene practices like brushing teeth, taking a shower, and putting on clean clothes, etc. Grooming becomes the last thing on their minds.
Mixed Dementia Treatment

To date, treatment for mixed dementia remains a challenge for medical practitioners.
However, there is a ray of hope for people with the illness because scientific studies show that it responds well to treatment options like:
Practicing Life-Long Heart-Healthy Lifestyle

Although this is not a treatment option per say, leading a healthy lifestyle can help delay or prevent the advancement of symptoms as the person with dementia grows older.
When talking about a healthy lifestyle, it means eating right.
This is where you get at least 3 or 4 healthy balanced meals. Avoid processed foods and too much sugar.
People with this type of dementia should also drink loads of plain water, stop smoking, cease drinking alcohol, and take part in exercise even when it is not too strenuous to get the heart beating as it should.
It also involves honoring doctor’s appointments so that a professional can check you out and give any advice necessary.
Different Types of Therapy

Some people with mixed dementia can benefit from various therapies.
These may include:
- Cognitive therapy
- Speech therapy
- Music therapy
- Aromatherapy
- Physiotherapy
- Occupational therapy
- Cognitive rehabilitation
- Reminiscence therapy, etc.
This is where the people with the illness take part in specific activities that help to stimulate thinking skills and how they interact with other people.
Most of the time these are usually group-based.
Facilitators often include games and music to make it more enjoyable.
Therapy can also assist with any movement issues to improve the overall quality and function of life.
It is best to have these done by a certified professional to avoid making things worse.
This is because it is not an easy task and caregivers need to be trained well on what to expect.
Drugs

Worth noting is that there is no medicine yet, for a person with a combination of two or more kinds of dementia.
Doctors may, however, prescribe various medicines in a bid to treat other underlying conditions that can cause damage to an individual’s blood vessels.
These include diseases like heart problems, stroke, diabetes, high cholesterol, and high blood pressure.
Controlling these risk factors is vital because it may protect the brain from harmful vascular changes.
Some drugs can also help with a variety of symptoms.
This is where a person takes medicine to relieve symptoms such as aggression, agitation, and anxiety.
Before giving the go-ahead to take any medicine, the doctor has to assess the person’s environment and health.
Palliative Care

Many people with mixed dementia end up in palliative care especially during the final stages of the disease.
This is the type of care that is accorded to people who have serious illnesses.
This can be done at home or in a health institution. It is quite different from the care that people receive when they are in the process of curing an illness.
The primary goal of this type of care is to enhance a person’s life quality focusing on the whole being i.e. mind, body, and soul.
Caregivers usually help persons under their care to become more independent while managing their daily lives.
They can also offer counseling and support when an individual needs these to help them feel better.
Final Thoughts

Thanks to advancements in the medical field, there are chances that as research continues to grow, mixed dementia will progressively be diagnosed and treated during life.
Experts are also coming up with new clinical trials for individuals to try and introduce new methods that will most likely manage, prevent, treat, or detect this type of dementia.