Previously referred to as precocious madness or premature dementia, dementia praecox was a term used to describe a chronic deteriorating psychotic disorder.
It was popularized by Emil Kraepelin, a German psychiatrist in 1896. The psychotic disorder that begins during late teens or early childhood is characterized by rapid cognitive disintegration.
Over time, the term “schizophrenia” replaced dementia praecox, and it remains the current diagnosis label.
Dementia Praecox: Definition, Causes and Symptoms
According to R.Warner, in the International Encyclopedia of the Social & Behavioural Sciences, schizophrenia is a psychosis – severe mental disorder where a person’s grasp of reality, emotions, judgment, thinking, and are affected resulting in severe impairment of functioning.
Causes of Dementia Praecox

To date, it is still not clear what causes schizophrenia exactly. Scientists, however, suggest that a combination of environmental, genetic, psychological, and physical factors can increase a person’s risk of getting the disorder.
Seeing that it is not easy to pinpoint the exact causes of schizophrenia, experts have identified some risk factors that are common with individuals who have the condition that includes:
Genetics

Dementia praecox tends to run in families even though there is no specific gene that has been identified to be responsible.
You will most likely end up with schizophrenia if your identical twin has it, the risk goes up by about 50%.
If both parents have it – the chances of getting it to go up by at least 40% or if a sibling or one parent has it – your chances of getting it is are around 10%.
Birth and Pregnancy Complications

Some studies indicate that a percentage of people who develop schizophrenia went through some complications before and during birth.
This accounts for factors like premature labor, low birth weight, and lack of oxygen during birth.
If your mother was malnourished when she was pregnant with you, you might end up with the disorder. Being exposed to a certain viral infection before you were born can also be a risk factor.
Drug Abuse

While drugs do not directly cause dementia praecox, research shows that drug abuse might increase the risk of developing the disorder.
Drugs like LSD, cocaine, or cannabis might trigger schizophrenia symptoms.
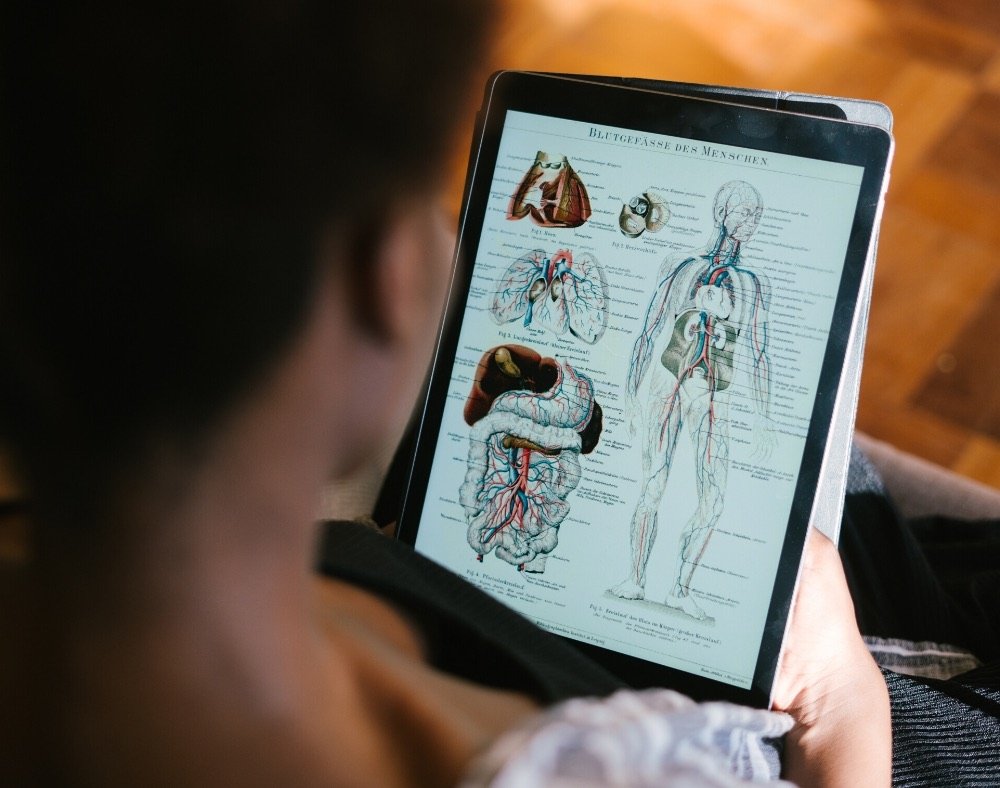
Chemical Imbalances in the Brain
Some experts believe that the imbalance of dopamine and serotonin, as well as other neurotransmitters, may be involved in the development of schizophrenia.
Trauma

The frequency of schizophrenia is also higher in adults who underwent different kinds of trauma in their childhood, such as physical or sexual abuse.
Triggers

These define things that can cause people who are at risk of developing schizophrenia. They include stressful life events such as losing a job, house, relationship, or a loved one.
Note that although these stressful events can be life-changing, they do not cause schizophrenia. Instead, they can trigger schizophrenia development in a person who is already vulnerable to the condition.
Symptoms of Dementia Praecox

A person usually experiences dementia praecox symptoms between the ages of 16-30. In some rare cases, young children also get a positive diagnosis for the disorder.
Schizophrenia symptoms are typically divided into three categories, namely: positive symptoms, cognitive symptoms and negative symptoms.
Let’s look at these categories individually below.
Cognitive Symptoms

The cognitive symptoms refer to the issues that arise when people with schizophrenia develop thinking problems. Most people with the disorder will have a hard time processing or understanding information, which can affect their ability to make decisions.
A huge percentage of affected persons will also have a hard time concentrating on something.
Some will also have trouble with working memory where they cannot use the information they have just learned. Because of all this, communication also becomes a problem.
Positive Symptoms

The positive symptoms are categorized as signs that showcase abnormal perceptions and delusions. These have a lot to do with the inability to determine what is real. This is where a person may have:
1. Hallucinations, false beliefs, or delusions: these are quite common with people with schizophrenia and can be related to auditory, visual, or any of the other human senses. These may become too real to a person to the extent that they are not even aware that they are ill.
Affected individuals might refuse to take medicine, thinking that it is poison or will subject them to adverse side effects.
2. Some people may also go through unusual thought disorders or disorganized and illogical thinking, which results in dysfunctional ways of thinking.
3. A certain percentage of people with the disorder may also showcase agitated physical movements.
4. Inappropriate behavior.
Negative Symptoms

Schizophrenia’s negative symptoms refer to the behavioral and emotional changes that the people with the disorder experience. These can include signs such as:
- Reduced facial expressions
- Flat affect which explains changes in voice tones
- Some persons with the disorder do not feel the daily pleasures of life
- Speaking very little
- Inability to begin or even continue activities
- Depression
- Mood changes
- Social withdrawal
- Absence of normal thoughts
- Loss of drive
There are other symptoms that some professionals use, which cannot fit into the three main categories. These include signs such as:
- Sleep disturbances
- Weight gain
- Restless leg syndrome
- Dropping performances especially for students
- Suicidal thoughts
Worth noting is that the dementia praecox symptoms start gradually develop at the onset of young adulthood and persist for as long as one lives.
The chronic condition also demands that most affected people go through lifelong treatment.
Closing Thoughts
Schizophrenia, which was known as dementia praecox, is among the most devastating neuropsychiatric diseases.
With this in mind, you should also note that experts are still working on ways to prevent and treat the condition.
There is a lot of hope that soon medics will be able to deal with the symptoms of the disease so that affected individuals can live “normal” lives functioning well in day to day activities while enjoying the little pleasures of life.