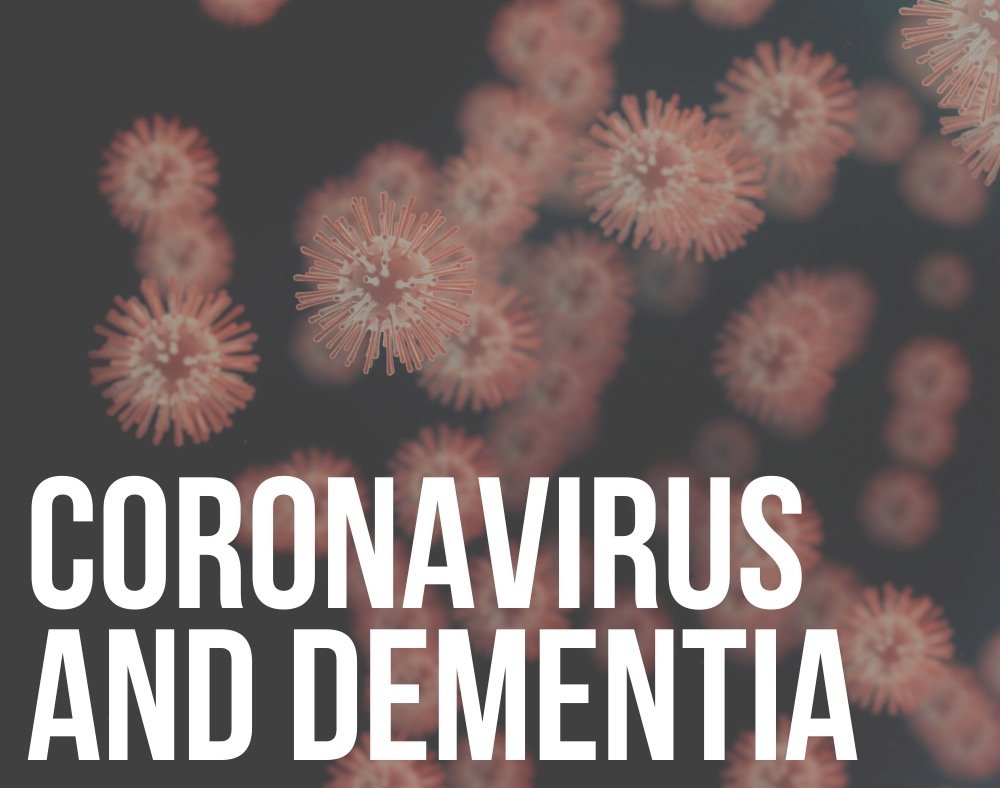
There is strong evidence developing in regards to exposure to air pollution and dementia risk.
Some researchers claim that small air pollution particles can enter the brain and contribute to the development of dementia.
Before looking at the possible link between dementia and air pollutants, first, check out what air pollution is.
Does Pollution Cause Dementia?
Air Pollution

Air pollution is made up of various components that may include:
- Chemical compounds
- Gases
- Tiny particles/ particulate matter
- Metals
Exposure to high levels of long-term exposure to air pollutants has been known to be harmful leading to the development of many health conditions that majorly affect the heart and the lungs.
Does Air Pollution Harm the Brain? (Different Studies)

One of the factors that led scientists to look into the relationship between air pollution and dementia is the existence of the magnetite particle in the brain.
These are particles that fill the air after the burning of fuel. The human brain also produces magnetite naturally.
A study conducted in 2016 confirmed that magnetite can make its way to the brain through air pollution. This was after studying the brain tissues of people from Manchester and Mexico City.

Researchers used a unique electron microscope to look at the surface properties of magnetite. They did this to prove that the brain did not produce the particles naturally.
Instead, they were produced by high temperatures.
The conclusion from the study was that it is possible that fine particulate material can enter the brain through the thin lining of the nose and the bloodstream as well.
Researchers observed that the particles were present inside amyloid plaques, which are the protein deposits common in the brain cells of a person with Alzheimer’s, one of the most common forms of dementia.
Magnetite can cause dementia
This is what led to the assumption that magnetite could be somehow involved in the development of dementia.
The study was, however not conclusive because it did not prove that magnetite was responsible for killing brain cells or the formation of the protein deposits.
There is a possibility that the particles might find their way into the brain and because of the organ’s waste disposal process find their way in the amyloid plaques.
In line with this Pektus, an assistant professor of clinical neurology working at Keck School of Medicine, led another study to try and add evidence linking air pollution and dementia risk.

The study focused on 998 female participants between the ages of 73-87.
The participants underwent two brain scans that were 5 years apart. Researchers studied the brains of the participants to give them a cognitive decline score.
They then combined the results with data on where the ladies lived with details about the pollution levels in the areas.
After analyzing this data, the researchers found that people who had higher exposure to fine air particle solutions were more likely to experience cognitive function impairments like memory problems.
A different study trying to prove the link between air pollution and dementia risk followed 130,000 people living in London for a couple of years.
The adults were aged 50 to 79. During the study period, at least 2181 people developed dementia. The results reported that the participants who were exposed to higher levels of air pollutants specifically nitrogen and fine particles from fossil fuel combustion had a higher risk of developing dementia.
The researchers stated that people living in London exposed to the highest levels of air pollution were around 11/2 times likely to develop some form of dementia.
Long-term exposure to air pollution can increase risk
A study conducted in 2017 studied adults for over a decade. The participants were quite many (about 6.5 million adults).
The study that was published in The Lancet found that the people who lived near high-traffic major roads were more likely to develop Alzheimer’s disease.
This was regardless of their socioeconomic and health status. The study claimed that about 6-7% of all dementia cases were attributed to exposure to air pollutants.
Another study followed residents in Stockholm, Sweden. They followed individuals who were exposed to air pollution at relatively low levels.
The research that was published in JAMA (Journal of the American Medical Association) found that even exposure to low levels of air pollution contributes to greater dementia risk specifically for persons who have heart diseaseshttps://readementia.com/signs-of-early-onset-alzheimers/.

Giulia Grande the lead author states that their findings suggested that air pollution plays a role in the development of dementia.
This is mainly through the intermediate step of cardiovascular illnesses and strokes. The researchers were studying about 3,000 adults for more than 11 years. The average age of the participants was 74.
Stroke and air pollution are most harmful
The study explained that while long-term exposure to air pollution was linked to dementia risk, this risk was higher for persons who suffered from a stroke.
About half of the dementia cases that they linked to air pollution exposure was explained by stroke. Researchers also noted that participants were residing in the Kungsholmen district where pollution levels are safely below international limits.
Scientists further extended their studies into mice. They found that there was a similar effect in the brain of mice after exposure to air pollution. The researchers exposed mice to air pollutants collected near busy roads.
This led to biological changes that usually cause brain damage and an increased level of protein amyloid.
This is still not enough to make a solid conclusion about the link between air pollution and dementia development.
It, however, shows that exposure to air pollution can lead to cognitive impairment. It is after the exposure brought forth symptoms like poor learning abilities, motor, and memory skills.
This is because, in the human brain, it is not automatic that amyloid protein on its own causes the development of dementia.
Closing Remarks
To give conclusive results on the issue of air pollution and dementia risk, scientists continue to conduct more studies to answer this question comprehensively.
The experts are taking into consideration pollution from different parts of the globe while using sophisticated techniques to try and establish if there is a direct link between air pollutants and dementia development.
Meanwhile, it is best for countries to start working on air quality to avoid some of the problems that are associated with air pollution.

















![Doll Therapy Dementia [Know the Pros and Cons] doll therapy dementia](https://readementia.com/wp-content/uploads/2020/03/doll-therapy-dementia.jpg)