It is vitally important to be armed with the right information about coping with dementia and behavior changes.
A person who has dementia goes through many stages and conditions in their lives, which might surprise you if you are unaware of them.
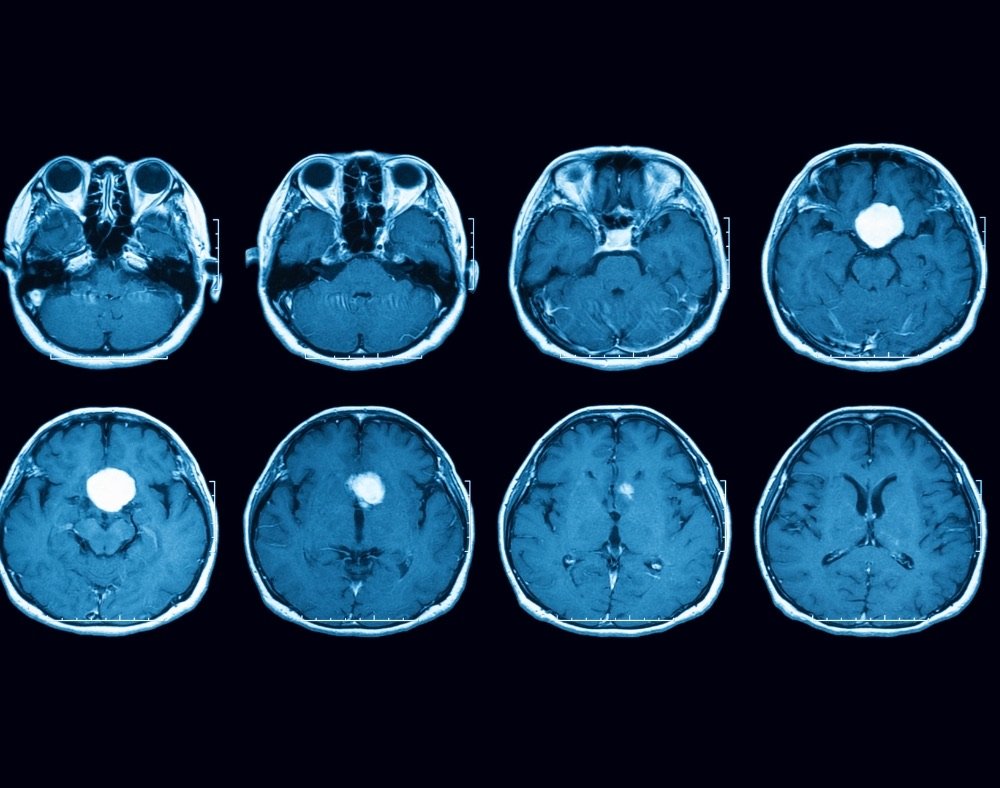
This is because the disease affects the brain triggering the loss of thinking skills, memory, communication, and many other aspects.
People with dementia may behave differently, especially during the middle to the final stages of the illness.
It mostly happens when an individual discovers that they are no longer in control of what is happening in and out of their lives.
This can cause a lot of stress not only for the person who has dementia but their loved ones and caregivers as well.
Depending on how the illness affects a person, there are various ways you may notice changes in how they conduct themselves.
Coping with dementia behavior changes
Here are a few common behavior changes examples and what to do when they occur.
Fidgeting and Restlessness

At some point, many people with dementia will develop restlessness behaviors. This is where an individual gets into the habit of pacing up and down without reason.
They may also start fidgeting without cause from the blues. Some will get agitated very quickly and may want to lash out at people all the time.
To take care of this issue, it is important that the person with dementia have a routine that they try and stick to on a daily basis.
This can help to keep them calm because they know what they do every day; thus, there is no need to fidget around or be restless.
Regular exercise has also been known to minimize restlessness.
When you notice that a person is always fidgeting, it is advisable to keep their hands busy with items like worry beads, or other items that they consider meaningful.
In the case of agitation, it may help to create a calm, soothing environment for a person who is triggered. Talking reassuring and lovingly to the person can help cool them down.
You may also want to consider something like a massage or any other activity that helps promote relaxation.
Wandering

Individuals who have dementia may start to walk around aimlessly.
There are multiple reasons why they can do this, such as medication side effects, boredom, or they want to look for someone or something.
Wandering can put someone in danger.
A person can even get lost since they may not be able to trace their way back home.
To prevent this from happening, there are a couple of solutions you can explore to help you in the journey of coping with dementia, like:
- Changing locks so that the person with the illness cannot easily get out of the house alone. It may seem a little mean, but there are times when you need to do this to keep the individual safe.
- Accompanying the individuals on walks or when they go to the shops is encouraged.
- Consider alarm systems, home monitoring systems, and tracking devices to enhance security.
- A person fond of wandering should wear an ID bracelet with the phone number of a relative. It comes in handy when somehow they get lost because someone out there can help them get reunited with their caregiver.
Hallucinations and Delusions

A person with dementia may, at times, develop false beliefs or delusions.
At times when a person with dementia experiences delusions, it can be paranoia.
For instance, a person might think that a spouse is being unfaithful, someone is stealing from them or people are out to get them.
Delusions can also be related to loss of memory. In such an instance, one might want to wake up and go to work even when they retired long ago.
Others may feel the need to take care of children even when they do not have any or get in a car and drive when they do not have a license.
When a person is going through these episodes, it is important to go in and see the doctor. The professional will be in the best position to rule out any medical issues.
Abrupt mental status changes can be brought about by pneumonia, constipation, urinary tract infections, dehydration, and other medical conditions.
At home, loved ones can try and distract the person with dementia with a conversation that sparks their interest.
Caregivers should not tell the affected individual not to be scared.
Instead, it is better to empathize with what they are going through and offer reassurance in a comforting and respectful manner.
You should also check out the environment that triggers hallucinations.
Be on the lookout for auditory and visual cues that may make a person feel threatened.
Eliminate or minimize shadows, objects, and noises that can be misperceived as disturbing or scary.
You should also try and identify the items that make the person feel secure.
It can be anything from a stuffed animal, photography, spiritual or religious item.
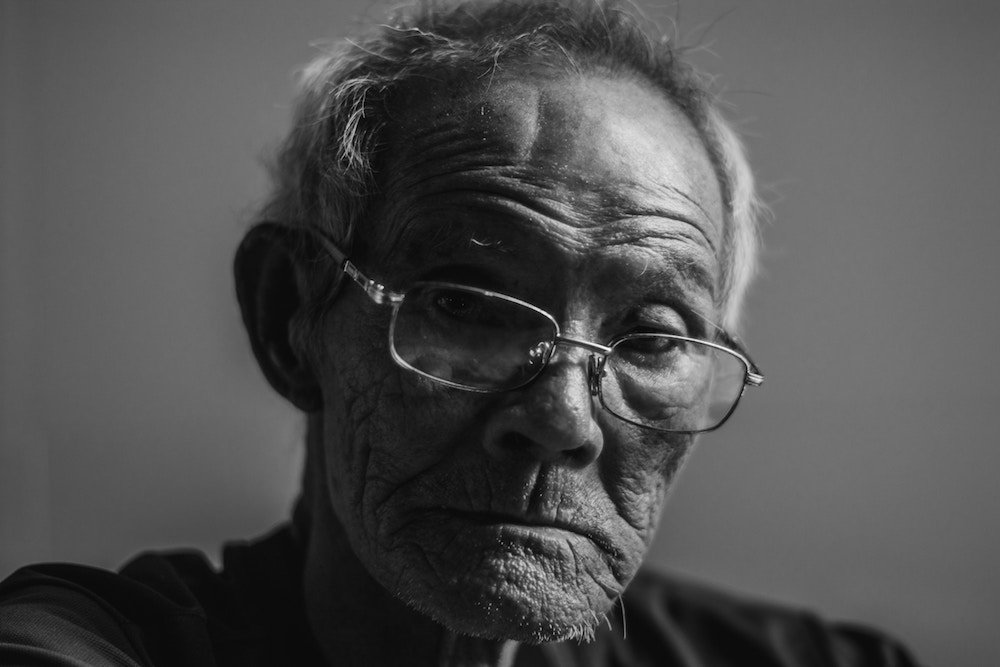
Depression

A high percentage of people with dementia also suffer from depression.
Getting to know if a person who has dementia also has depression can be quite challenging since both conditions have similar symptoms.
A medical professional can, however, conduct a thorough evaluation to diagnose depression.
Thankfully, depression does not have to be a huge burden to someone coping with dementia.
Treatment is available and it normally involves a combination of counseling, medication and continuing reconnection to people and activities that bring bliss.
As a caregiver do not be the one always to tell a dementia patient to “try harder,” “snap out of it,” or “cheer up” because this rarely helps.
People who have dementia and depression cannot simply get better by themselves. They need a lot of professional help, reassurance, and support.
Sleep Problems

Many senior dementia patients complain about sleep all the time. Poor sleeping habits, certain medications, alcohol use, and stress are some contributing factors that lead to disturbed sleep.
Restlessness, agitation, and confusion can also affect how a person with dementia sleeps.
Studies reveal that sleep issues are one of the reasons individuals with dementia have to stay in nursing homes.
So that a person can function well, they must get enough quality sleep.
Some tips that can help with ensuring a person with dementia does not end up struggling to get a shut-eye include:
1. Keeping away from alcohol because it contributes to confusion and also increases anxiety.
2. Limit beverages and food that contain high caffeine levels, especially later in the day because it can lead to sleeplessness.
3. Plan the days in a way that incorporates numerous activities. When you fill-up the days with meaningful activities, it can lead to exhaustion so that a person sleeps well at night.
It can be anything from taking walks, exercising, or participating in involving hobbies. However, you must be careful not to overstimulate the individual with dementia.
This will only lead to disorientation, which is not healthy for one’s sleeping time. It is also important to limit nap time as this can also affect how a person sleeps.
It may also help to come up with a bedtime routine that mainly focuses on relaxing activities such as giving the person with the illness a massage or listening to soft music.
Hoarding

Some people will dementia will pick up a habit along the way where they cannot let go of their possessions.
As a person who is coping with dementia, several things that can lead to the development of this behavior like isolation, loss, fear, and memories of the past.
To help the individual deal with this, you can try and keep them busy with other things. For instance, you can give them a box full of different items that they can sort.
You can also learn where a person hides the things they want to hoard and remove them without the individual noticing.
You must be very careful with this so as not to agitate them further causing more problems.
Closing Remarks
There is no set of rules that you should follow when it comes to coping with dementia.
To best meet the challenges, you need to use a lot of compassion, creativity, patience, and flexibility to try and make the best out of a rather challenging situation.
Some things must be put into consideration when dealing with a person who has dementia, like:
1. It is not possible to change the person because it is a brain disorder that shapes how they behave.
2. Rather than try and control behavior, it’s best to try and accommodate the new changes in the best possible way.
For example, if a person wants to sleep on the floor, do not force them to climb on the bed. You can place a mattress on the floor instead to make them feel as comfortable as possible.
3. When there is a sudden behavior change, it is always wise to consult with a doctor. This is because some problems may come about because of various underlying medical reasons.
A person with dementia may be in pain or be experiencing side effects from the medications they are taking.
Sometimes, hallucinations or side effects may be caused by treatment or medication that is helping to manage the condition.



























 neurological dementia signs” width=”1000″ height=”788″ class=”alignnone size-full wp-image-11129″ />
neurological dementia signs” width=”1000″ height=”788″ class=”alignnone size-full wp-image-11129″ />