We’ve dealt many times with negative thinking and dementia. We also found several studies revealing the possible link between the two.
Thus conducted this article that will help you and your loved ones with the impact of negative thinking.
Does Negative Thinking Influence Dementia?
Researchers from University College London conducted the research suggesting that repetitive negative thinking also known as perseverative cognition is linked to a higher number of harmful protein deposits in the brain which is linked to cognitive decline.
Subsequently, this INCREASES the risk of developing dementia.
Natalie L. Marchant the lead investigator of the study said that they were prompted to carry out the research based on the fact that anxiety and depression are known as dementia risk factors in mid- and old-age.
The research revealed that certain thinking patterns implicated in anxiety and depression could be the reason individuals experiencing disorders are MORE LIKELY to get dementia.

She further explained that chronic perseverative cognition patterns over long periods of time could increase the risk of dementia.
However, there was no evidence showing that SHORT-TERM setbacks increase an individual’s risk of developing dementia.
More details of the novel study below.
Participants and Duration of the Research
The researchers observed hundreds of participants who were above 55 years over a four year period.
All the participants were in good cognitive and physical health and had a parent or sibling with Alzheimer’s disease.
The authors of the study looked at two cohorts of participants.
The first came from the PREVENT- AD (Pre-symptomatic Evaluation of Experimental or Novel Treatments for Alzheimer’s disease) research project.
Other participants were drawn from IMAP+ (Multi-Modal Neuroimaging in Alzheimer’s disease) study.
Both studies involved 360 participants.
Research nurses conducted DETAILED medical examinations before enrolling the subjects to ensure they were eligible for the study.
During this time, participants were asked to respond to questions that indicated how they normally felt about various negative experiences.
The queries were primarily centered on patterns that are usually observed in repetitive negative thinking.
These include worrying about the future or thoughts of past events.
The research team also assessed the cognitive function of the subjects including language, attention, and spatial cognition.
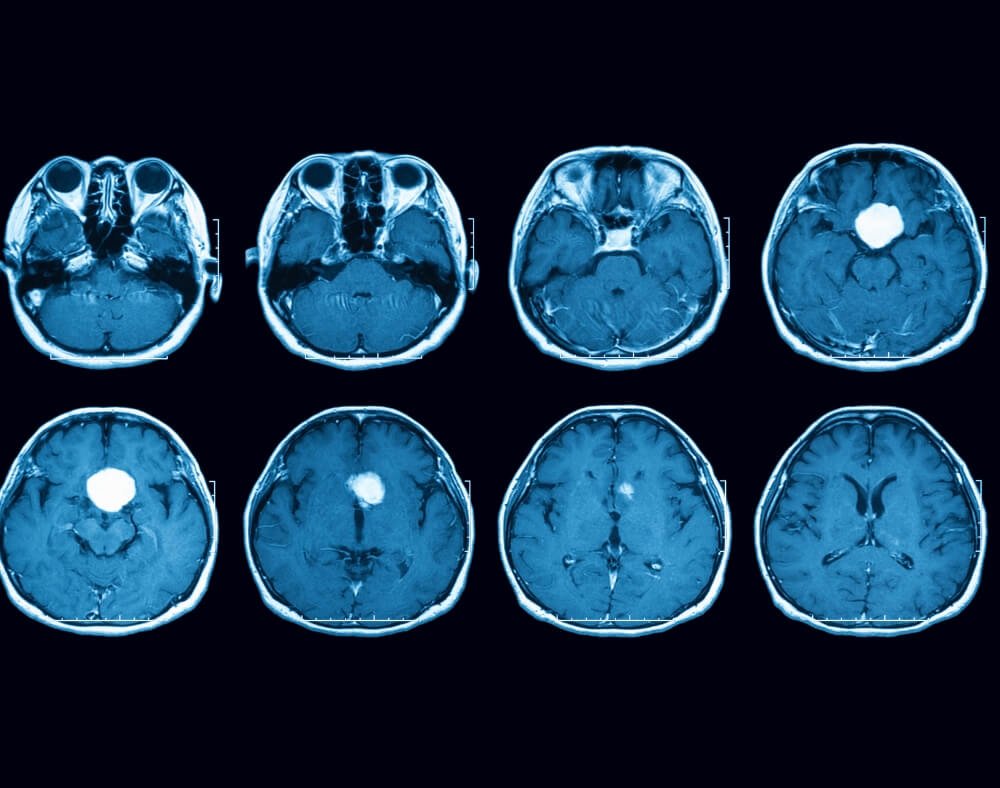
In the quest to find out if there is a relationship between negative thinking and dementia, 113 participants had PET scans.
These were done to measure the amount of amyloid and tau deposits in the brain.
Alzheimer’s disease is linked to an excessive accumulation of these two proteins in the brain.
Results of the Study
Researchers found that the participants who demonstrated HIGHER LEVELS of repeated negative thinking patterns had more memory and cognitive decline.
Additionally, the group of participants also had more tau and amyloid deposits when compared to the ones who did not have repetitive negative thinking patterns.
Marchant concluded that repetitive negative thinking could be one of the new risk factors for dementia.
It could contribute to the development of the illness in a unique manner.
Researchers also noted some limitations of the study.
While there may be an association between repetitive negative thinking and dementia, the casual relationship between the two is still not clear.
Authors believe that perseverative cognition contributes to the development of Alzheimer’s by ELEVATING an individual’s stress levels.
Furthermore, the experts could not ignore the fact that early signs of Alzheimer’s disease could also lead to repetitive negative thinking.
Tips for Avoiding Repetitive Negative Thinking
Seeing that there could be a link between negative thinking and dementia, it is possible that the risk of developing the illness can be reduced by being more positive.
Researchers are currently taking up projects to see whether interventions such as meditation, mindfulness training, and targeted talk therapy can help REDUCE repeated negative thoughts.
Dr. Gael Chetelat co-author of the study stated that people’s thoughts have a biological impact on physical health.
It can either be negative or positive.
He believed that mental training practice CAN PROMOTE positive thinking.
The doctor advised individuals to take care of their mental health.
He says that this should be a major public health priority.
It is important for people’s well-being and health in the short term and can reduce the risk of dementia.
Responding to this, Dr. Jacob Hall a neurologist at Stanford Health Care said that experts must use scales to determine what is considered normal or abnormal when it comes to negative thoughts.
Positive thoughts increase the quality of life

This is because some negative thoughts are considered to be a normal part of life.
Hall said that there it is still not clear whether perseverative cognition causes, accelerates, or is just associated with Alzheimer’s disease.
He, however, noted that a positive mindset is associated with tons of benefits.
He went further to state that healthier thinking patterns can lead to a higher quality of life reducing the risk of multiple health problems including dementia.
There is no doubt that a positive outlook is great for the mind, body, and brain.
Previous research supports the hypotheses of the study indicating persons who are more positive usually have a better shot at avoiding death from cardiovascular risks than pessimistic people.
A study conducted in 2019 revealed that more positive individuals enjoyed GREATER protection from stroke, heart attacks, and other causes of death.
Moving Forward
Based on the results of the study, researchers hope for more studies on the link between negative thinking and dementia.
We can use the findings to develop effective strategies to IMPROVE the quality of life.
These can lower the risk of people developing dementia by curbing repetitive negative thoughts.