We want to share with you some of Alzheimer’s disease facts and figures to truly understand how much impact this disease has.
There are only a few more diseases that cause more deaths than Alzheimer’s disease.
Thus it’s important to be familiar with its global effect, so you act AS SOON AS POSSIBLE and get appropriate treatment.
10 Alzheimer’s Disease Facts You Should Know
1. Approx. 6.2 million Americans have Alzheimer’s disease
This is a startling statistic. It is even more amplified by the fact there are aging adults who are currently undiagnosed and not receiving treatment.
Worldwide, there are already around 50 million people with AD or other types of dementia. The number keeps on expanding by millions a year.
2. Alzheimer’s disease cannot be reversed.

There isn’t a cure for Alzheimer’s disease. The progressive symptoms of the disease cannot be halted or prevented. Researchers are searching for answers and more viable treatment options.
Planning for palliative care and supportive environments must be an integral part of the conversation for patients and their families.
3. Dementia and Alzheimer are not the same.

Many times, we hear these two terms interchanged as a synonymous disease. They are not the same, but rather dementia is a subset of Alzheimer’s disease.
Dementia is defined as a decline in mental cognition and ability. It is a blanket term for a set of symptoms associated with compromised brain function.
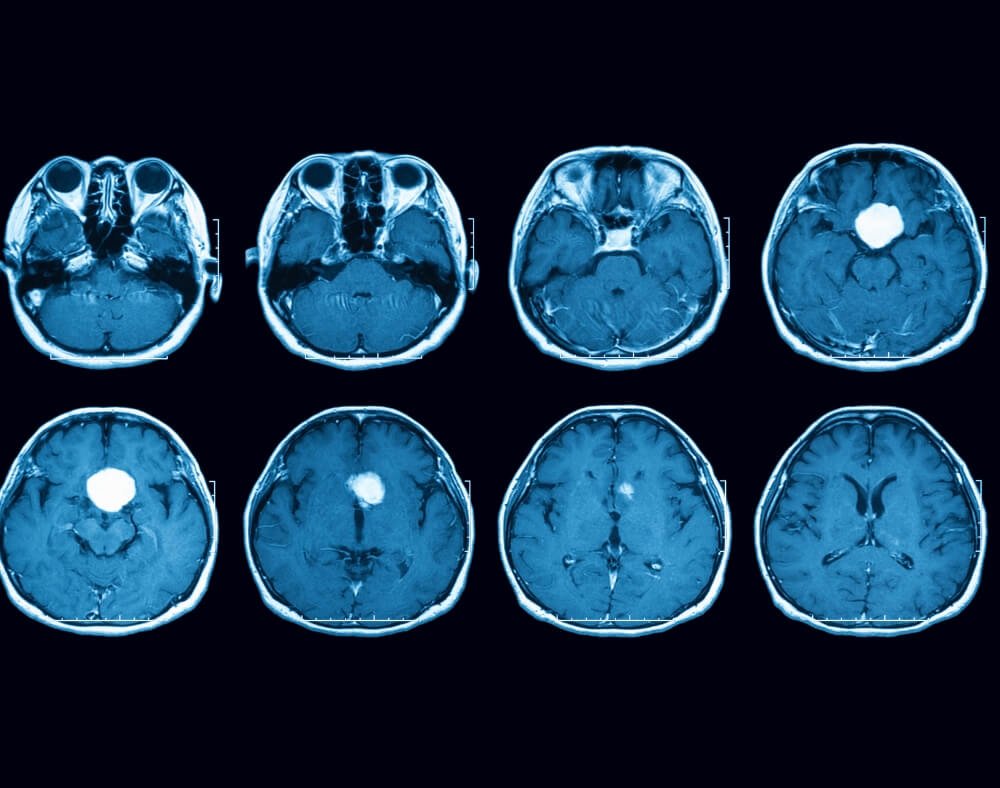
Whereas, Alzheimer’s disease is classically defined as when brain cells progressively die over time that results in memory loss, brain function, cognitive function, and behavior.
Alzheimer’s disease is almost always confirmed at the time of death after analyzing brain tissue.
The clinical findings that assist to diagnose Alzheimer’s disease are tangles or plaques, which act as evidence of damaged brain cells.
Additionally, the causes vary for patients suffering from forms of dementia.
4. There are Six Main Types of Dementia
- Vascular Dementia
- Dementia with Lewy Bodies
- Frontotemporal Lobar Dementia
- Mixed Dementia
- Huntington’s Disease
- Alzheimer’s disease
5. Alzheimer’s disease does not have a cure.

Currently, there are approximately 132 agents in Alzheimer’s disease-related clinical trials across the globe.
Researchers are tapping into RNA-type clinical data that has been made available due to the increases in technology and molecular chemistry.
The objectives are to gain knowledge for the purpose of developing more effective treatment strategies and interventions.
6. Alzheimer’s disease ranked as the 6th leading cause of death in the United States.

Wellness efforts have helped decrease preventable diseases and conditions that stem from high blood pressure, obesity, exercise deficiency and poor nutrition.
However, systemic and genetically derived blood and health conditions rank high among those contributing to early morbidity.
Diseases and conditions that are associated with the brain are some of the most difficult to prevent and have zero cure.
Therefore, Alzheimer’s disease is among those that affect don’t have much of a preventable precursor aside from aging.
7. Causes and Risk Factors for Alzheimer’s disease
- Age
- Family History
- Genetics
- Brain Injury
- Vascular Health (heart disease, stroke, HBD)
8. Women are more likely than men to be affected by Alzheimer’s disease.

Several leading experts are opening the conversation about why women are more likely than men to be diagnosed with Alzheimer’s disease.
Researchers cite that women in their sixties are two times more likely to be diagnosed with Alzheimer’s disease than breast cancer.
Some of the speculations point to genetics, longevity, and life experience. The questions are out there, and researchers are diving deep to answer them.
We need to stay tuned and see what is revealed in the future regarding possible links between female related risk factors for this disease and others.
9. Vulnerable Populations at Risk for Alzheimer’s disease: Latinos and African Americans.
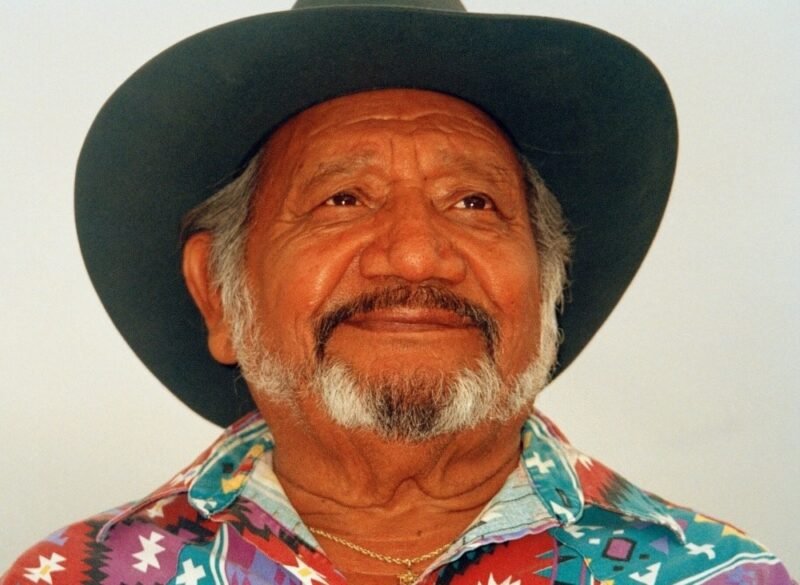
It is estimated that by 2030, Latinos and African Americans will make up as much as 40% of the 8.4 billion people projected to suffer from Alzheimer’s.
10. Life Expectancy Varies by Individual Case.

The prognosis for patients with Alzheimer’s disease is assessed in the scope of three distinct stages; early stage, middle stage and late stage.
What we know about this disease, is that the presentations and hallmark symptoms are consistently represented in one of these stages.
The disease, unfortunately, is very progressive. While living with Alzheimer’s is possible for an undetermined number of years, the degenerative process isn’t reversible.
The goals for caregivers and families are centered around supportive care and safety protocols.
Early Stage Common Symptomology:
- Difficulty naming common things
- Forgetting things that were read or written moments before
- Misplacing valuables and money
Middle Stage Common Symptomology:
- Unstable Moods and Irritability
- Slight Incontinence
- Problems choosing weather appropriate clothing
- Getting lost/wandering aimlessly
- Forgetting the date, address, appointments, etc.
Late Stage Common Symptomology:
- Trouble communicating
- Requires 24-hour supervision
- Vulnerable to illness and infection
- Compromised physical abilities
Conclusion: What does the future hold for Alzheimer’s patients
As a degenerative disease, Alzheimer’s can spark a hefty amount of uncertainty and fear especially, as we begin to age.
It is hard to know what care and treatment options might be available for future generations.
Research efforts are aggressive, and many strides have been made in the way of early detection, drug therapies, and advanced knowledge.
Collectively, the medical community and information hubs like this one serve to present current updates on Alzheimer’s disease news and research.
Bonus: About Alzheimer’s disease facts
Alzheimer’s disease facts- history and hope.
Alzheimer’s disease (AD) was named based on the work of Alois Alzheimer. In the year of 1906, Dr. Alzheimer noticed usual brain lesions and clumps taken from a mentally ill woman.
Her condition, which was designated as rare, included symptoms including memory loss, language problems, and unpredictable behavior.
Following her death, an autopsy was conducted.
Dr. Alzheimer found many abnormal clumps (now called amyloid plaques) and tangled bundles of fibers (now called neurofibrillary, or tau, tangles).
These were the foundation elements that now represent the widely accepted scientific biomarkers for Alzheimer’s disease.
The brain is something that even researchers agree there is much they just don’t yet understand.
However, through decades of active clinical trials, patient-case anomalies, and advanced technology, the knowledge base is ever-expanding.
We should even be encouraged by this.
Every notable clinical finding serves to introduce new avenues for treatment and early diagnostic techniques.
More importantly, it gives way to enhanced potential for genetic interventions.