Numerous research studies confirm that there is a link between dementia and high blood pressure.
High blood pressure also known as hypertension is a chronic condition where the force of blood against the artery walls becomes too high causing various health problems including strokes and heart attacks.
Hypertension is known to cause progressive brain damage.
Blood pressure usually measures the force that is applied to the arteries as blood is circulated by the heart around the body.
Normal blood pressure should read about 120/80 mmHg. Hypertension is constantly above 140/90 mmHg.
Common risk factors for high blood pressure include an unhealthy diet comprising mostly salty foods, lack of exercise, excessive alcohol consumption, being obese or overweight, taking steroid medication, drinking lots of caffeine and kidney disease.
Also, everyone in the family with a history of hypertension is at risk, as well as those of Caribbean or African descent.
Dementia is a general term that is used to describe problems with memory, problem-solving, language, and other thinking abilities that end up interfering with a person’s day-to-day life.
The disease is progressive implying that the symptoms will become worse over time.
Research on Dementia and High Blood Pressure

The World Alzheimer Report 2014 states that several studies observing large groups of individuals demonstrated that people with hypertension especially in mid-life were at high risk of developing vascular dementia one of the most common kinds of dementia later on in life.
The subjects were between the ages of 15-40 while mid-life was characterized by people between the ages of 40-64.
Vascular dementia occurs when there is an inadequate flow of blood to the brain which denies the organ essential nutrients and oxygen it needs to function properly.
People with hypertension are at higher risk

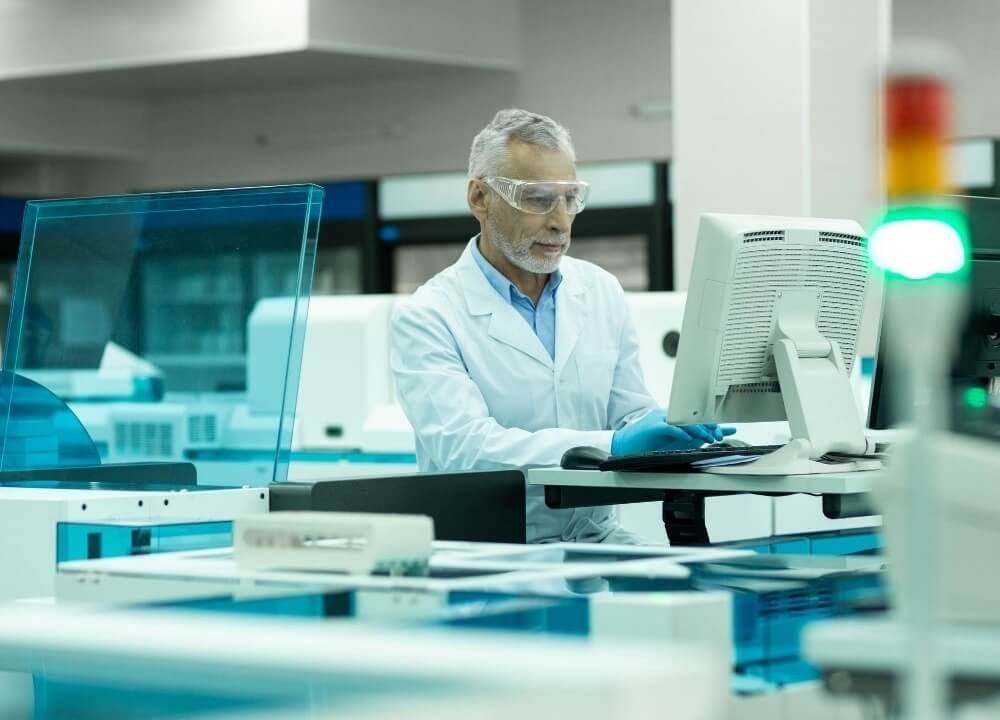
A study published by Oxford University Press in Cardiovascular Research also reports that persons who have hypertension are at a higher risk of getting dementia.
For the first time, the research also reveals that doctors can conduct an MRI to detect neurological damage for persons with high blood pressure before dementia symptoms occur.
Researchers came to this conclusion after subjecting individuals between the ages of 40-65 to undergo a 3 Tesla MRI scan at the Regional Excellent Hypertension Centre of the Italian Society of Hypertension of the I.R.C.C.S.
The participants of the study did not have a dementia diagnosis or any structural damage.
The subjects also underwent clinical examinations to know their hypertensive status as well as damage to the target organ.
They were also subjected to an MRI scan to identify any microstructural damage.
The results indicated that hypersensitive participants had major alternations in 3 specific white matter fiber tracts.
The group also scored worse in cognitive tests and decreased performances in memory, speed, and learning-related tasks.
This goes to show that it is possible to detect changes before a person starts showcasing symptoms. Medics can then offer medication that will prevent further deterioration in regard to brain function.
Hypertension medication and dementia

Another study worth mentioning about dementia and high blood pressure was conducted at the John Hopkins University.
Experts analyzed previously gathered data to report that persons taking hypertension medication were half as likely to end up with Alzheimer’s (the most common cause of dementia) when compared to the people who do not take the drugs.
Constantine Lyketsos, director of Memory and Alzheimer’s treatment at John Hopkins explained that people who do not have Alzheimer’s but are taking blood pressure drugs were less likely to develop dementia.
He went ahead to say that individuals who got dementia from Alzheimer’s and were taking specific antihypertensives were likely to experience slow or halt progress.
He concluded that it was still not clear where this connection arises.
It can either be from better management of blood pressure or some medications that may have some properties that interfere with some of the processes that relate to Alzheimer’s.
Women with high blood pressure are more like to get dementia

A sex-specific study reveals that women who experience hypertension in their 40’s are 73% more likely to get dementia later in life when compared to the ladies who did not have high blood pressure.
This was in a bid to determine how dementia strikes women and men differently.
Experts who conducted the study said they adjusted the results for other risk factors that can also lead to dementia including diabetes, smoking, and obesity which held true for all races.
This, however, was not the same case for men even though hypertension was more common among the male fraternity. The study that was published in the American Academy of Neurology journal observed more than 7,000 individuals.
The participants went through blood pressure checks at the age of 33 and again at 44 in the 60s and 70s. Researchers began to follow up to see the persons who developed dementia in 1996.
The results indicated that ladies who had hypertension in their 30’s did not have a higher dementia risk as compared to those with high blood pressure in their 40’s.
How Hypertension Affects the Brain

There are several ways high blood pressure affects the function of the brain. One of them is that over time, hypertension causes strain on the arteries.
This makes the artery walls become stiffer, thicker, and narrower a condition known as arteriosclerosis.
When this happens, the brain is deprived of important oxygen and nutrients which results in damaged brain cells that negatively affect the functioning of the brain.
Hypertension is also one of the major stroke risk factors.
One of the major reasons that cause strokes is the blockage of arteries in the brain which is usually a result of hardening arteries.
A stroke can also occur when an artery in the brain burst causing bleeding in the organ. Strokes can result in post-stroke or stroke-related vascular dementia.
When talking about dementia and high blood pressure, it is also important to mention that hypertension can damage small blood vessels in the brain.
This can affect the parts of the brain responsible for memory and thinking.
Closing Remarks
Even though the link between vascular dementia and high blood pressure is quite apparent, there is still no proof that lowering blood pressure can help to prevent the development of dementia.
More research needs to be done to identify the link between hypertension and dementia to see if anything can be done to prevent or treat dementia.