After extensive research, we look into the commonly-asked-question of whether or not can a CT scan show dementia.
It IS POSSIBLE to detect the condition by watching for telltale signs in loved ones or yourself.
The cause of action, in this case, is to visit a physician right away so that they can perform brain imaging procedures TO DETECT the progressive neurologic disorder.
That begs the question, can a CT scan show dementia?
When Doctors Prescribe Brain Scans?
Your physician might suggest that you get a brain scan to identify underlying problems causing mental conditions or affecting your general wellbeing.

Typically they are used to detect tumors, strokes, as well as other problems THAT CAN spark dementia that may appear on brain scans.
The cortex of the brain appears overly wrinkled and it has gyri (ridges of tissue) which are separated by sulci (valleys).
Individuals with cortical atrophy experience the progressive loss of neurons which in turn causes the thinning of the ridges and the sulci to grow wider.
When brain cells continue dying, the brain’s fluid-filled cavities (ventricles) expand and occupy the available space.
In turn, they become LARGER than normal.
These structural changes within the brain are also aspects that BRAIN SCANS CAN IDENTIFY.
How Do CT Scans Show Dementia?
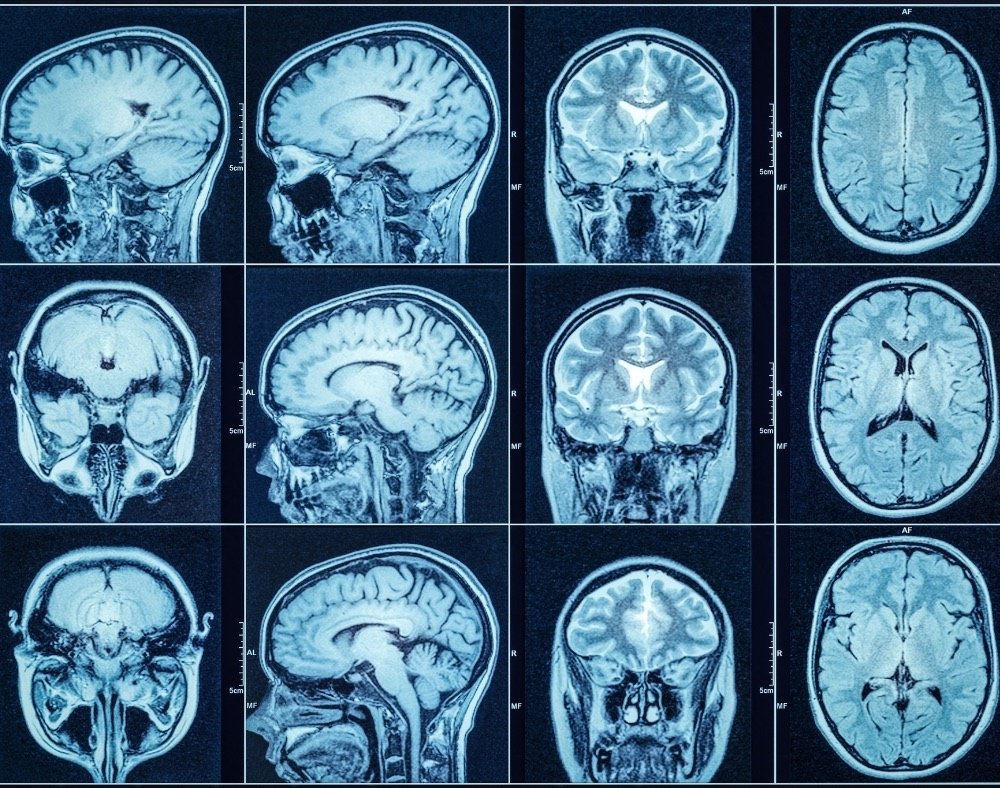
The most common types of brain scan you might encounter are magnetic resonance imaging (MRI) and computed tomographic (CT) scans.

Doctors regularly recommend MRIs and CT scans when they examine someone they suspect has dementia.
CT scans detect brain structures through X-rays and the procedure can reveal evidence of ischemia, brain atrophy, and strokes.
The procedure also picks up on PROBLEMS like subdural hematomas, hydrocephalus, and changes that affect the blood vessels.
As implied, MRIs make use of focused radio waves and magnetic fields to detect the presence of hydrogen atoms within the body’s tissues.
MRIs ARE BETTER at diagnosing brain atrophy and the damage that subtle ischemia or incidents of small strokes cause to the brain.
Thus, MRI is normally the first test a person undergoes and CT second.
Other Imaging Options That Can Diagnose Dementia
Several other brain imaging procedures exist. Each can help detect dementia in different ways.
EEGs (electroencephalogram)
EEGs (electroencephalograms) are sometimes used on people who have suspected seizures, which accompany some types of dementia.
The procedure involves placing several electrodes at different points on the scalp to check for abnormalities in the brain through the recorded patterns of electrical activity.
The electrical activity shows instances of cognitive dysfunction that plague parts of the brain or the entire organ.
People with MODERATE to SEVERE cases of dementia present abnormal EEGs.
The procedure can also identify seizures, which 10% of people with Alzheimer’s are reported to experience.
Functional Brain Imaging
Functional brain imaging procedures are not often used as diagnostic tools. But they help researchers in the process of studying people with dementia.
They include functional single-photon emission computed tomography (SPECT), MRI (fMRI), magnetoencephalography (MEG), and positron emission tomography (PET) scans.
Nowadays, they have a hand in the EARLY DETECTION of dementia.
fMRI measures metabolic changes happening within the brain using strong magnetic fields.
SPECT scans reveal blood distribution within the brain. This aspect is responsible for discovering increased brain activity.
PET scans pick up on blood flow, glucose, and oxygen metabolism, and if amyloid proteins are present within the brain.
MEG scans record the electromagnetic fields that the brain produces through neuronal activities.
Additional Tests to Treat and Manage Dementia
Once an individual is diagnosed with dementia, the next step that follows is helping them understand how the condition will affect them and how to manage it.

Several other medical assessments exist to help physicians understand how the condition affects a specific person. And also help families, as well as caregivers, figure out the best course of treatment for the individual.
Did you HEAR of the peanut butter test?
Neuropsychological Testing
Neuropsychologists and psychologists who have specialized training can also prescribe neuropsychological tests to detect dementia.
The process involves WRITTEN and ORAL tests that can take several hours to complete.
They use these methods to assess the cognitive functions of the person suspected to have dementia.
It helps them figure out if (and which) certain areas are impaired.
The tests assess aspects like vision-motor, memory, comprehension, reasoning, coordination, and writing abilities.
Physicians may administer additional tests to find out if the person in question is SUFFERING from mood problems or dementia.
Functional Assessments
Dementia is a cognitive disorder that affects the afflicted person’s daily functioning in different regards.
Objective assessments can establish what a person is STILL ABLE to do versus what they can no longer do in light of the condition.
Family members are asked to fill questionnaires that provide details about the person’s daily life in terms of the activities they are able to perform.
They generally note the tasks related to daily living that their loved one can complete partially, successfully, or have challenges in fulfilling.
The test also reveals the stage of Alzheimer’s afflicting the person undergoing the process. This, in turn, helps physicians and their loved ones charter the RIGHT COURSE of treatment.
The information also helps caregivers particularly in the case of someone who also suffers from other health problems like poor vision or arthritis that aggravate the degenerative condition.
Psychosocial evaluation
Social workers conduct psychosocial evaluations designed to assist the person’s family to make arrangements for their care.
They discuss the financial, physical, and emotional impacts that come from having a loved one suffer from the range of progressive brain degeneration disorders.
They also help with the process of organizing community services that can benefit the person as well as offer suggestions about alternative living arrangements if necessary.
Clinical Trials To Detect Dementia
Many people are taking part in RESEARCH STUDIES and clinical trials helping implement new medical approaches, equipment, drugs, and other treatment options in general.
People who take part in these studies gain access to advanced diagnosis or treatment options. It can help them manage the condition significantly.
Can a CT Scan Show Dementia? Conclusion
The bottom line is that CT scans and other brain imaging procedures CAN HELP diagnose dementia at any stage.
Combined with other assessments available, an individual battling the condition can get help early enough to manage it.
Families of people with dementia and caregivers can also access crucial information from these tests. They help in the process of caring for the individual.