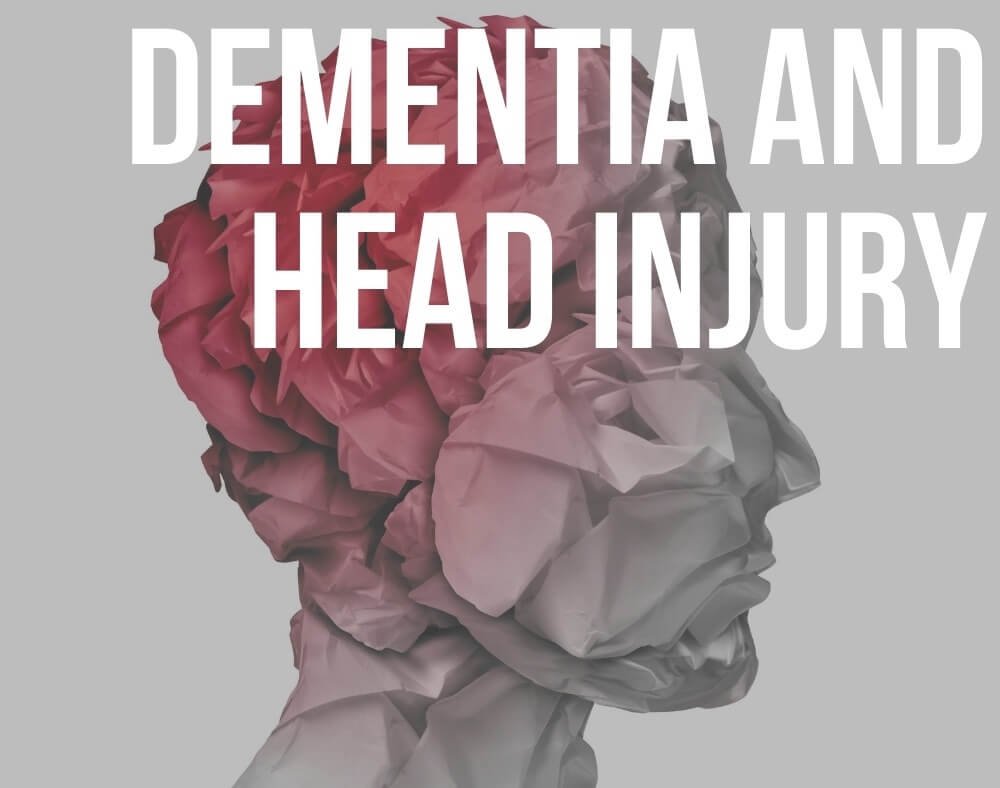
The potential between increased risk of dementia and traumatic brain injury has become a pressing issue as scientists try to find the link between the two.
This is mostly because the immediate effects of head injury can include symptoms that are similar to those of dementia.
These include signs such as memory loss, confusion, and changes in speech, personality, and vision.
Relationship Between Dementia and Traumatic Brain Injury
Depending on the severity of the head injury the symptoms can clear up fast, last a long time, or fail to go away altogether.
Keep in mind that symptoms a person experiences after an injury usually do not become worse over time which is usually the case with dementia.
Dementia affects about 47 million people worldwide and we expect the numbers to double in the next two decades.
Over 50 million people across the globe experience traumatic brain injury yearly.
Causes of TBI

This usually occurs when external forced disrupt the normal functions of the brain. Leading causes of TBI include falls, assaults, and motor vehicle accidents.
Research, however, notes that certain types of head injuries may increase the risk of someone developing different types of dementia.
Two primary factors seemingly affecting a person’s risk include the severity of the injury and the age when the injury happened.
Some studies suggest that more severe head injuries might increase the risk of developing Alzheimer’s disease (AD) which is one of the most common causes of dementia.
The risk also increases for persons who experience head injuries when they are older say 55 years and above.
Repeated mild injuries also increase the risk of having problems with reasoning and thinking in the future.
Brain injuries after 55 are risky

Check out essential details of a study that has been done to try and figure out the link between the risk of dementia and traumatic brain injury.
One of the larger studies reported that the risk of dementia as well as that of Alzheimer’s is significantly higher in persons who have experienced TBI than in those who have no history of traumatic brain injury.
The study that was conducted in Denmark observed almost 2.8 million participants and they began in 1977.
The large study population involved a 36-year follow-up where researchers gained access to a uniform healthcare system that tracks the severity and numbers of traumatic brain injuries.
Among the millions of participants, the research indicated that 4.7% have at least one diagnosis of traumatic brain injury.
With the first TBI diagnosis, 85% had been categorized as mild while the rest were characterized as a skull fracture or severe. 4.5% of the persons who were 50 years and above developed dementia from 1999 to 2013.
From this group, 5.3% had experienced at least one TBI when the scientists were conducting their observations.
The average age at first dementia diagnosis was recorded as 80.7 years. The findings of this research were published in The Lancet Psychiatry on 10th April.
Dementia risk is higher in those with TBI history
The experts in the study concluded that the overall dementia risk in people with a history of TBI was 24% higher than those who did not have a history of traumatic brain injury.
They reached this conclusion after accounting for other risk factors of the neurodegenerative disease.
Severe traumatic brain injuries accounted for an increased risk of 35% while mild TBI increased the risk by 17%.
Men also have a slightly higher increased risk of dementia development when compared to women with traumatic brain injury histories at 30% versus 19%.
Jesse Fann the lead author of the study and a professor of behavioral sciences and psychiatry at the University of Washington School of medicine said that the relationship between the risk of dementia and the number of brain injuries was very clear according to the research.
Men are more likely to develop dementia after TBI

The study also indicated that the risk of dementia also increased based on the number of traumatic brain injuries.
Five or more TBIs increased the risk by 183%, four TBIs increased dementia risk by 51%, while the risk increased by 33% for two or three TBIs.
Fann also explained that if someone had a brain injury in their 20’s chances of developing dementia increased by 60% in their 50s.
The researchers nonetheless clarified that the findings of the study do not suggest that everyone who sustains traumatic brain injury will end up developing dementia in his or her later years.
Fann hoped that the findings will help people with histories of TBI to change their behaviors towards other dementia risk factors.
This includes quitting or limiting the use of tobacco and alcohol consumption, taking part in regular physical exercise, treating illnesses like depression, diabetes, and hypertension, as well as avoiding obesity.
He also suggested that people who have suffered traumatic brain injury need to get an evaluation from medical doctors to get immediate treatment for any persisting issues.
Fann stated that some cognitive rehabilitation strategies might help decrease cognitive deficits that relate to brain injury.
Not everyone with traumatic brain injury will develop dementia

Co-author Jakob Christensen an associate professor of neurology at Aarhus University Hospital in Denmark stated that severe traumatic brain injury is more prevalent in young people.
He went ahead to explain that there is a concern that this also increases the risk of developing dementia in younger people.
Fann warned children and parents to be aware of the risks of traumatic brain injury that contact sports present.
The authors of the study recommended heightened efforts to prevent TBIs, especially for the younger generation.
They said that strategies need to be put in place to ameliorate the impact and risk of dementia relating to traumatic brain injury.
Conclusion
Many studies looking into the relationship between increased risk of dementia and traumatic brain injury are targeting participants of contact sports such as hockey, football, boxing, and soccer as well as military veterans.
These are people who end up experiencing traumatic brain injuries in their line of work.
The researchers acknowledged that more research is still needed to find out who is at the greatest risk of developing dementia as well as other factors that contribute to this risk.