We found it essential to understand the connection between poor balance and dementia when carrying for grandparents.
As a consequence, we combined our experience with studies to bring you this EXTENSIVE OVERVIEW of balance loss in dementia.
Persons living with dementia normally experience poor balance at several stages.
Some people will start losing balance when walking or standing before other dementia symptoms start to develop. This may be an indication that the individual is at risk of developing Alzheimer’s.
Understanding Balance Loss in Dementia (+ Tips)
Researchers from the University of California conducted a study that identified a strong correlation between the risk of dementia and poor balance. They used 2 types of physical performance tests: the 13-foot walking test and the standing balance test.
The professionals discovered that poor balance recorded the strongest association with dementia incidences.
It can also be a sign that an individual is already suffering from another type of dementia.
A person may exhibit loss of balance differently depending on the type of dementia they have.
For instance, for Alzheimer’s disease (AD), loss of balance is TYPICALLY a sign of the late stages of the illness.
When seniors are experiencing poor balance and they are not showcasing memory loss or any other early dementia warning signs, vascular dementia may cause poor balance.
Causes of Poor Balance for Individuals with Dementia

Individuals experience poor balance and dementia for a variety of reasons and some of them are:
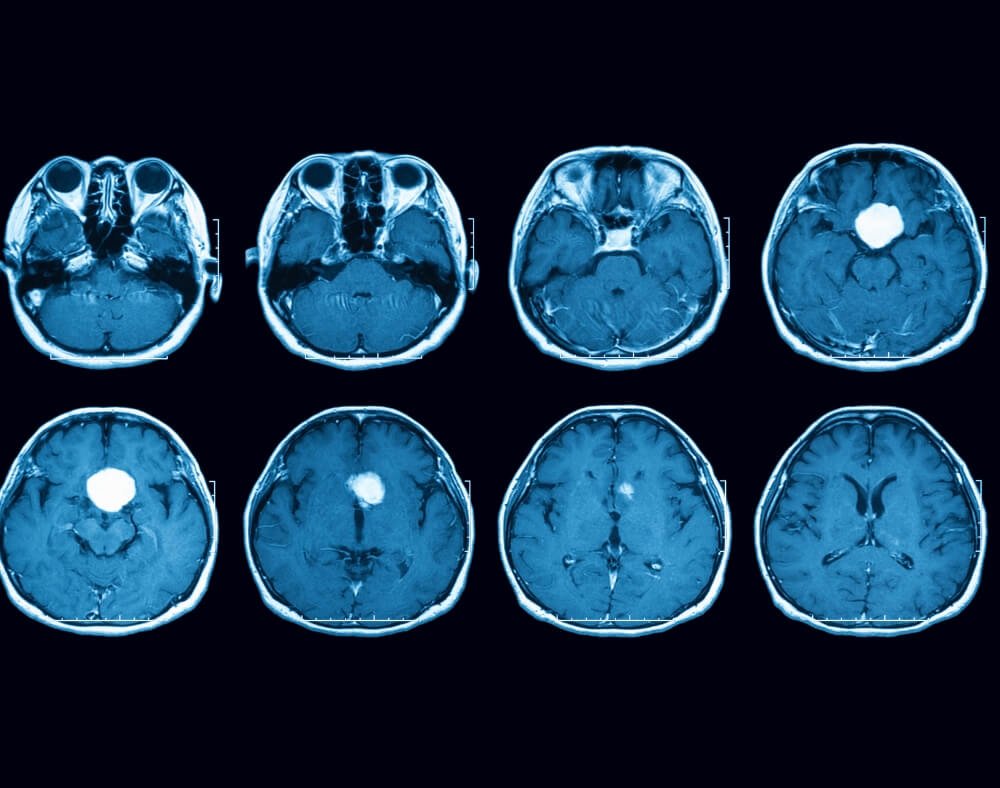
Damaged Brain Vessels
If an individual has vascular dementia, it means that damaged blood vessels are blocking or reducing the flow of blood to the brain. This can cause problems with balance, movement, and weakness on one side of the body.
This is mostly because the illness NEGATIVELY affects the cerebellum. The cerebellum is the part of the brain that is responsible for controlling body movements.
It is located close to the back base of the skull. Because dementia is a progressive illness, the symptoms only get worse over time.
Alzheimer’s disease
AD is another reason people will experience poor balance. This normally happens in the later stages of the illness.
As the brain cells continue to deteriorate, neural communication in the body also becomes worse. This causes people with Alzheimer’s to have challenges seeing, walking, and processing information about the physical environment.
All this ends up affecting a person’s balance.
A majority of people will start changing how they walk as they START shuffling their feet rather than lifting them with each step.
This makes it very hard to walk, a loss of balance, and falls also become more likely.
Medications
Many drugs that seniors take cause light-headedness or dizziness which can increase the risks of falls.
These can include medications prescribed for blood pressure or the ones that individuals take to relieve other symptoms they may have.
Consulting a doctor may help confirm whether the medications a person is taking are causing loss of balance.
The professional will then CHANGE the drugs to options with less or no interactions.
Note: Hearing aids and cochlear implants that are rooted inside the ear could also be the cause of dizziness and vertigo which may explain why a person has balance issues.
Identifying Balance Problems

Several signs may be an indication that a person had poor balance such as:
- Walking unsteadily
- Bumping into things
- Shuffling of feet instead of lifting them
- Stooped posture
- Turning through small steps instead of pivoting on heels
Dealing with Poor Balance and Dementia
When a person with dementia is experiencing issues with balance, there are a few tips they can work with to help cope with the changes.
Early Detection

An early dementia diagnosis may help LIMIT the severity and impact of poor balance.
It is, therefore, important for anyone who suspects having any type of dementia to consult a doctor as soon as possible.
This increases the chance of catching the illness early.
Home Improvements
If the person with dementia is experiencing poor balance and is still leaving at home, it may be important to make some adjustments at home to create a more secure environment.
These include the installation of walk-in-baths/ showers or wet rooms to make bathing easier and safer.
Installation of anti-slip floors, handrails, seats, and low threshold entry points can also help.
Try and ENSURE that the home is easy to navigate as this reduces accidents while ensuring affected persons retain their independence.
By creating a dementia-friendly home, you may be able to leave someone with dementia home alone for longer.
Working Out

If a person is able; it helps to engage in exercises like leg lifts, Tai Chi or riding a stationary bike.
Exercises are important for people with poor balance and dementia because it not only increases flexibility but it also enhances memory and lowers anxiety.
Low-impact workouts can also help strengthen leg muscles, improve balance, and maintain bone density.
Mobility Aids
The use of mobility aids like walkers and canes can help people with dementia maintain balance and become more comfortable when walking or standing.
Remember to talk to a physical therapist or doctor before getting any mobility aid so that the experts can GUIDE YOU on the most effective aid to purchase.
Balance and Dementia Closing Thoughts
Caring for a person with dementia means that the caregiver at some point may have to deal with poor balance and dementia.
It is important to understand what causes balance issues and come up with effective ways of dealing with the problem.
This way, the person with the progressive illness gets to lead a more COMFORTABLE LIFE and reduces the risk of falls, pain and other accidents.