An in-depth look at the differences and similarities between cortical and subcortical dementia and what you should do about it.
Also known as a major neurocognitive disorder, dementia is a group of symptoms that causes problems with memory, reasoning, and thinking.
It occurs when parts of the brain responsible for memory, decision-making, language, and learning are diseased or damaged.
The illness mostly affects elderly persons who are above the age of 65.
Some persons will, however, receive dementia diagnosis when they are younger.
There are over fifty causes of dementia the most common ones being:
- Degenerative neurological diseases: these include different sclerosis type, Alzheimer’s disease (AD), Huntington’s disease, and Parkinson’s disease.
- Traumatic brain injuries
- Nervous system infections
- Vascular disorders
- Long-term abuse of drugs or alcohol
- The build-up of brain fluid, etc.
Cortical vs Subcortical Dementia
Depending on the part of the brain that has been affected, a majority of dementias are either considered to exhibit cortical or subcortical patterns.
Initially, subcortical dementia was described in 1912. However, the term was not used until 1970.
Cortical dementia, on the other hand, accounts for the highest number of dementia cases (between 60-80%).
Various studies indicate that there are some prominent differences between cortical and subcortical dementia.
Both qualitative and quantitative differences exist across several cognitive domains like memory, visuospatial abilities, executive functions, attention, and semantic knowledge.
Let’s look at some of the disparities between the two groups of dementias below.
Definition

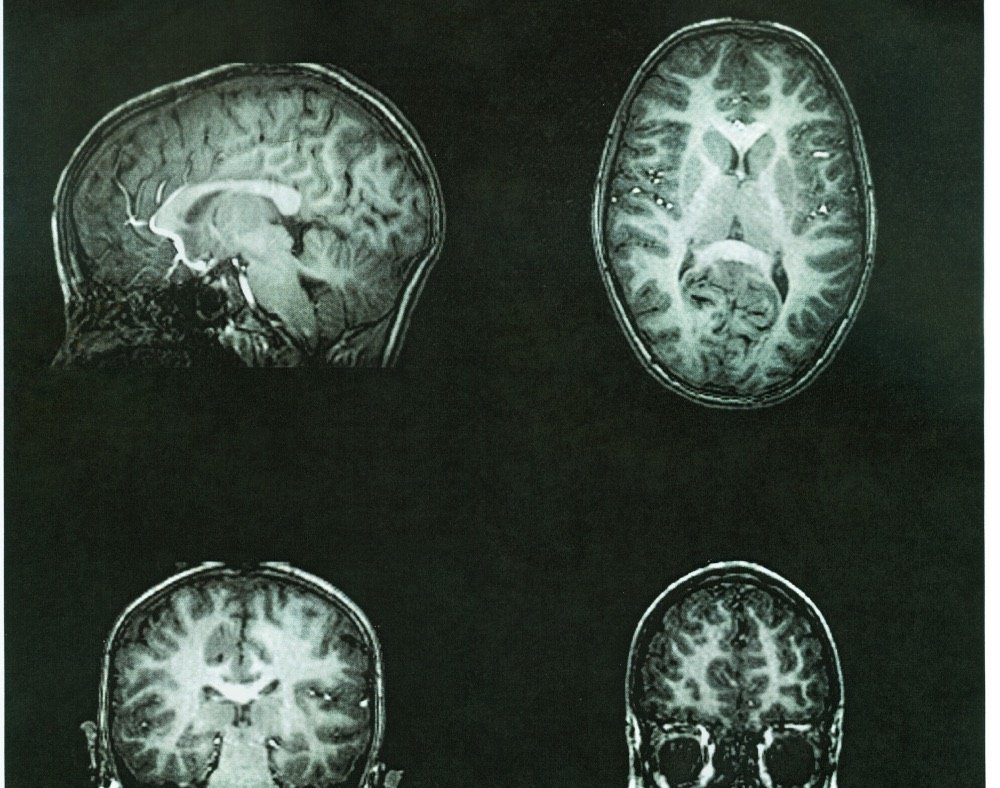
Cortical dementia describes the types of dementia that develop as a result of disorders that affect the cerebral cortex in the brain.
This is the outermost layer of the brain responsible for several essential functions like language, memory, creativity, abstraction, emotion, attention and judgment.
The illnesses that are progressive in nature starts to cause changes in the brain before the symptoms start showing up.
Experts believe that the illness brings about an increase in the number of lesions in the brain, which then leads to complications like personality changes and loss of memory.
Subcortical dementias represent the types of dementias that showcase themselves without any language or memory problems in individuals who have Alzheimer’s disease.
Disorders that affect the section of the brain that is below the cerebral cortex cause this dementia.
The regions of the brain that this type of dementia affects include the midbrain, striatum, thalamus, and striatofrontal projections.
In most cases, persons who get subcortical dementia display challenges with concentration, attention, and motor function.
Causes Cortical and Subcortical Dementia
Cortical dementia as aforementioned, occurs where there are problems with the cerebral cortex.
Additionally, it is primarily associated with the gray matter in the brain, which mainly consists of nerve cells.
Persons who develop this type of dementia experience serious memory loss issues where they cannot understand language or remember words.
Examples of cortical dementia include Creutzfeldt-Jakob and Alzheimer’s disease.
Subcortical dementia, on the other hand, is brought about when there are problems in the part of the brain located under the cortex.
This is mostly associated with the white matter of the brain that predominantly consists of axons that are in charge of transmitting signals.
Individuals who have this type of dementia typically show changes in their ability to start activities and speed of thinking. HIV, Parkinson’s and Huntington’s disease are possible causes of this dementia type.
Some studies also suggest that prolonged alcohol abuse may be the cause of subcortical dementia.
This is because persons who are diagnosed with alcohol dependence have a significant reduction in the brain’s white matter and the weight of the brain also becomes lighter.
Features of Cortical and Subcortical Dementia

Both dementias showcase different features that further explain their main differences like:
Basic function deficit
With cortical dementia, you can expect specific deficits like aphasia, which is an impairment of language that affects comprehension or production of speech and the ability to write and read.
Apraxia affects motor function and agnosia, which affects the ability to process sensory information.
Subcortical dementia presents progressive supra-nuclear palsy, a syndrome that can lead to severe problems with eye movement, balance, swallowing, mood and walking, etc.
Memory impairment
Persons with cortical dementia will often experience learning deficits and poor recognition. Individuals with subcortical dementia do not go through severe memory loss issues.
Caregivers and loved ones can use cues to help the affected individuals recall information without too much difficulty.
Motor Symptoms

Cortical dementia does not showcase any motor symptoms, especially in the early stages of the illness. Motor speed also remains relatively healthy, but it might change at a later course.
Problems with motor symptoms are common with subcortical dementia that presents extrapyramidal symptoms that can include continuous muscle contractions and spasms also known as dystonia, motor restlessness, rigidity, slowness of movement, and tremor amongst others.
Speech
Individuals with subcortical dementia, for the most part, will have normal speech while it may be slow or abnormal in cortical dementia cases.
Symptom Profile
Cortical and subcortical dementia have different sets of symptoms.
Clinically, cortical dementia exhibits symptoms that are suggestive of abnormalities with various cortical functions like amnesia and language issues.
With subcortical dementia, the symptoms will manifest mainly as poor abstraction, issues in recall, mood disorders, and problems with strategy formation. Other symptoms to look into include:
Memory

Memory dysfunctions tend to occur in both groups of dementia.
Studies, however, propose that the nature of memory impairment is different in subcortical and cortical dementia.
Cortical dementia showcases more severe memory loss, which is depicted by difficulties in recalling information and learning new details.
When it comes to subcortical dementia, things are not black and white.
While there is evidence of challenges with procedural learning, the impairment is not uniform in regards to all kinds of perceptomotor learning.
For example, a person who has Parkinson’s disease might have issues with skill or habit learning but have no problem in intact learning tasks such as artificial grammar and dot pattern prototype.
Memory loss patterns also come into play when differentiating these two forms of dementia.
With cortical dementia, recent literature indicates that memory impairment evolution happens in a temporal gradient, which results in progressive or extensive remote memory loss.
This is especially true for autobiographical memory.
On the contrary, the memory loss pattern in subcortical dementia is considered to be a lot more diverse. The specific type of dementia will determine the memory loss pattern.
For instance, persons who have Parkinson’s disease normally have challenges when dating events in the past.
Note that memory decline is faster in Parkinson’s dementia than in AD as reported by Selective Reminding Test and Boston naming test.
It is also important to point out that with subcortical dementias, learning impairments are subject to correction with the use of more prominent aid recognition cues.
Executive Functions

Executive functions usually involve the frontal lobes and other subcortical structures. This means that it is only natural for executive function problems to be present in both subcortical and cortical dementia.
This, however, happens at a different rate.
AD is normally characterized by the impairment of various executive functions like problem-solving and concept formation.
Persons who have cortical dementia will experience impaired elementary calculation skills earlier than those who have subcortical dementia.
Persons with cortical dementia also remain alert for more extended periods than those with subcortical dementia.
Language
Several studies indicate that the language problem is often seen in cortical dementia.
Individuals with Alzheimer’s disease exhibit several progressive language issues. These normally start with an inability to recall names of familiar objects before it deteriorates to terminal language syndrome.
Prognosis of Cortical and Subcortical Dementia
The prognosis of cortical and subcortical dementia also significantly varies. Because different types of dementias fall under these two categories, multiple factors commonly affect prognosis.
Among these include general health, age of onset, and other illnesses that the person suffers from. These can affect not only prognosis but life expectancy as well.
Treatment

Currently, there is no specific cure for both cortical and subcortical dementia.
However, a majority of the disorders that are listed for the two groups of dementia will respond to appropriate treatment.
These can include different types of medication and other alternative therapies that can help to slow down the progression of the illness.
Lifestyle changes can also help to improve the life quality of people who are experiencing different types of dementia.
Closing Thoughts
Understanding the differences between the two main groups of dementias is essential because it helps to create a better understanding of how the brain behaves regarding neurodegenerative illnesses.
This can also help medics improve the ability to differentiate multiple dementia disorders clinically.
There is also a need for more clinical studies that will examine the differences between subcortical dementia and cortical dementia. These are bound to give a clearer picture of the factors that distinguish the two forms of dementia.
The Alzheimer’s Association indicates that about 90% of the information available about dementia has been discovered in under twenty years.
Experts in the industry continue to do more research, tests, and studies on this disease that affects millions of people in different parts of the globe.
Fresh information may continue to roll out detailing the differences or similarities of cortical and subcortical dementia so that people can get a better understanding of these illnesses.