We will look at the most common frontotemporal dementia symptoms as they can vary quite a bit from person to person.
Some are pretty similar to other types of dementia, but the treatment can be different due to the disease affecting different areas of the brain.
But what exactly is frontotemporal dementia (FTD) and why it occurs?
First and foremost, frontotemporal dementia is an umbrella term for different conditions. We know three main types of FTD:
- Behavioral variant FTD
- Progressive non-fluent aphasia
- Semantic dementia
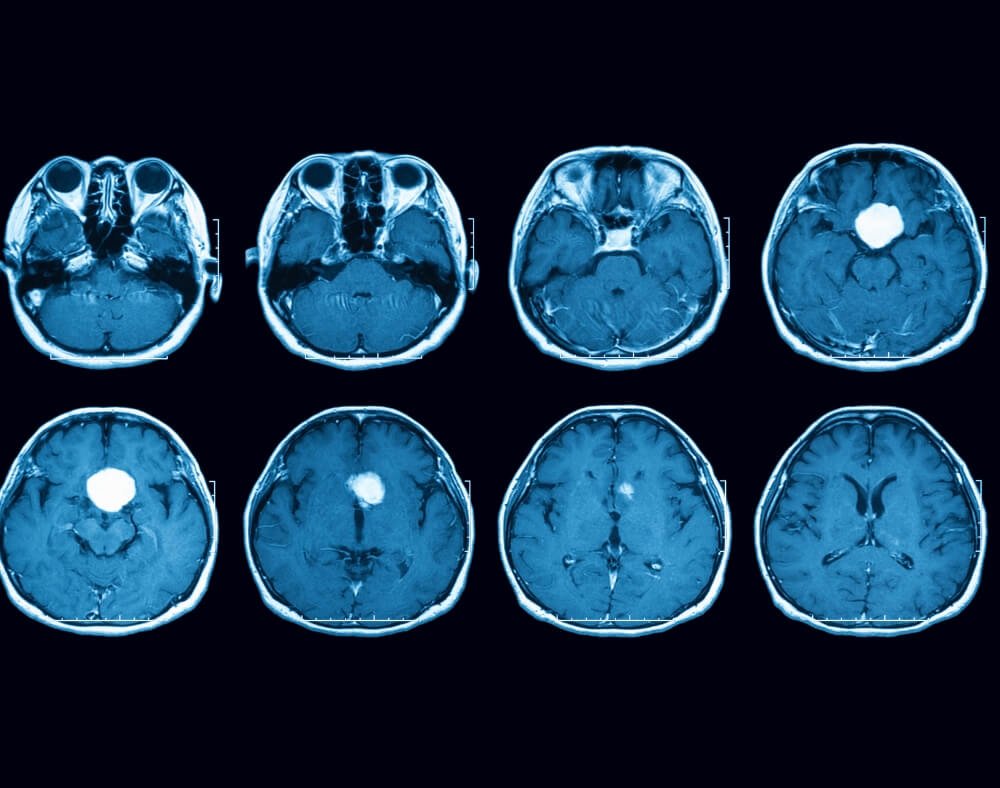
Moreover, FTD increases nerve loss in the frontal and temporal lobes of the brain. The former is the area behind your forehead and the latter the section behind the ears.
A person with FTD mainly shows signs that are related to behavior, personality and communication/language which worsen over time. In the later stages of frontotemporal dementia, a person needs 24-hour care.
Today, we will investigate different frontotemporal dementia symptoms that caregivers, friends and family members should be aware of.
Note that an individual can have a mixture of two or more symptoms which cause difficulty prescribing the right treatment.
At the time of writing this, FTD and any other type of dementia still have no cure. However, there are different behavioral and lifestyle changes that we can implement to reduce the risk of dementia.
12 Frontotemporal Dementia Symptoms and Signs
1. Apathy

It is easy to notice this change in a person that was once an outgoing, active and friendly individual with a lot of friends and rich social life.
However, all of a sudden, they lose interest in other people, events and friends. A person with frontotemporal dementia, as well, starts to lose motivation for hobbies and other activities that he or she once loved.
When you ask this person why they do not do activities anymore he or she just doesn’t have the motivation to do anything anymore. Also, a person doesn’t have any bad feelings toward friends and society just doesn’t want to be connected with them anymore.
As a result, they like to spend time alone. An apathetic person has an absence of interest in social, spiritual, physical, emotional and family life.
2. Lack of sympathy and empathy

A person with frontotemporal dementia symptoms puts himself first. He or she has difficulties to see and understand the needs of other people (his caregivers, family members, friends).
They show less personal warmth and love even to his wife or her husband. Besides, a person can show no interest in their children or grandchildren.
Which can be difficult to understand and to accept for family members.
Moreover, a person can be less socially active or doesn’t show any interest in the social environment, events or celebrations.
This behavior can make the person appear harmful or selfish and has to be understood as illness and not as an unfriendly attitude or hostility.
3. Repetitive behavior

A person can develop a behavior pattern or gestures that are repeated many times in a day. A person can also start hoarding stuff and doesn’t want to throw away their belongings.
Especially disturbing are used wipes, old food and empty food packing. Common frontotemporal dementia symptom is when a person repeats phrases and questions multiple times in just one hour.
Some behaviors can become almost ritualized and cannot be interrupted. If a caregiver doesn’t do something like the ritual a person with frontotemporal dementia developed, the person with the condition can get very angry and upset.
For example, if the food isn’t served like the person with frontotemporal dementia expects, he or she can become a nuisance.
4. Poor planning and trouble making decisions

Another of the frontotemporal dementia symptoms is with organizing and planning. Difficulties may be first noticed at work if a person is still employed. A retired person can show a lack of organizing and managing their finances.
As an example, house expenses and bills aren’t paid in time, or the wrong amount is paid. A person can be confused with the understanding of the value of money and can waste it for unnecessary things.
Another common frontotemporal dementia symptom is the difficulty of making decisions. More importantly, the decision to actually executing an activity or task. On the other hand, they might have trouble considering what should be the best thing to do in a particular situation.
It is important for a person to have a caregiver, family member, friend, that helps him to understand the value of the decision and what should be the best for them to do.
5. Loss of communication

A person with frontotemporal dementia can experience loss of expression. Communication can be hard to understand with a lot of errors in grammar. A person can be really slow at speaking and experiences difficulties to find the right word and meaning of a sentence.
You can notice that an individual is leaving out small words in the sentence such as the, from, to, etc. It becomes challenging to understand what they try to say when the words are mispronounced or wrong.
You have to be attentive to understand a person with frontotemporal dementia who has symptoms of loss of communication.
Don’t argue with a person about errors in grammar and just listen attentively and connect the story in a whole tale with a sense of its potential.
After some time, it gets easier to understand the meaning even if the words are wrong and are missing.
6. Memory

Common frontotemporal dementia symptom is connected with memory. One of the first signs is when a person’s vocabulary gets inadequate.
Additionally, a person can be confused about everyday objects and doesn’t recognize items that he/she uses, eats and see every day.
A person can be asking about the meaning of familiar words (what is “glass,” what is “an apple,” etc.). Similarly, a person doesn’t recognize familiar people, family and friends.
Loss of short-term memory can be noticed when a person doesn’t recollect what he ate one hour ago, if he already was in the shop that day or if he/she had any family visits in the morning.
7. Agitated behavior
The more that the brain becomes damaged, the more agitated or aggressive a person can become. In this stage of frontotemporal dementia, a person can be hard to understand, has limited communication and poor focus.
He or she can become angry or aggressive by the smallest things that do not go according to their plan. This could be a simple misunderstanding in conversation.
Or if a family member thinks or wants to prove that the person with dementia is behaving weird or inappropriate.
Try to understand that the brain is damaged and that person can’t act and behave as he/she used to.
A person starts to do everyday things in a routine and gets upset if the routine is broken. In this stage, a person will likely need a full-time caregiver.
8. Poor personal hygiene

A person with frontotemporal dementia symptoms can start to diminish personal hygiene, and doesn’t want to take regular showers, clean teeth and wash clothes.
Clothes seem to a person with frontotemporal dementia always clean and he/she does not want to change them even if they are full of stains.
Showers start to become unnecessary and complicated. Plus, the cleanliness of the bathroom and living space becomes poor and dirty.
It is necessary that family members check if the bathroom and kitchen are clean and safe to use if a person is living alone.
9. Movement problems

Common symptoms of frontotemporal dementia are those that relate to the movement of a person. A person can develop tremors and can’t stop trembling, which leads to incapability to take care of his/her basic needs in everyday life tasks.
A problem can start with an eating disorder due to the difficulty of swallowing of food and liquids.
Not enough food can lower energy and consequently, lack of active movement.
With no activity, human muscles start to weaken which can lead to problems with balance. A person can easily fall and lose stability while standing.
Try to help a person with movement problems to stay active and walk at least ten minutes a day if possible so that some muscles will stay fresh and preserved.
10. Change of personality

The characteristics and personality of a person with dementia can change with a damaged brain. Alterations can be so severe that the person that you once knew doesn’t exist anymore.
We simply have to accept a new personality that an individual has developed.
Remember that the changes, especially if they are negative, are due to the disease. A person with frontotemporal dementia is not trying to hurt you, or be negative and ungrateful.
Set reasonable expectations and don’t demand behavior that a person with frontotemporal dementia cannot provide.
If personality changes are so severe and sudden that you cannot cope with them, contact a physician for help.
11. Sudden speech problems

It is more likely that a person with FTD will have issues with speech compared to those with Alzheimer’s disease. This results in one of quite common frontotemporal dementia symptoms.
A person has trouble not just remembering names and words but making sense when they speak and understanding others. They even tend to use more general words when describing things, even people, like it, he, she, etc.
Moreover, difficulty also occurs when it comes to reading.
To sum up, when an older adult starts to have speech problems, you better take him or her to see the doctor as early as possible. In some instances, complete loss of speech may also become a thing.
12. Weird eating habits

One widespread frontotemporal dementia symptom is the development of weird eating habits.
All of a sudden, they start to crave foods that they never before liked. Moreover, overeating is an almost popular act in people with frontotemporal dementia.
That’s not all. It is also quite natural that they begin to desire sweet foods, primarily carbohydrates.
Last but not least, one of the signs of their weird eating habits is the fact that they begin eating inedible, heck, contaminated objects. You, as a caregiver or loved one, should pay close attention to what the older adult is doing.
And if they need more attention during morning or later hours, that’s what you would want to try to take care of.
Final Thoughts – Frontotemporal Dementia Symptoms
There are a range of Frontotemporal dementia symptoms, to include changes in behavior and personality to language difficulties and impaired organizational function.
Recognizing these early signs is important to allow for timely diagnosis and access to the right care. By having an understanding and awareness of these symptoms, families can navigate the challenges posed by frontotemporal dementia.
By doing so, they will be better able to manage the condition and provide the appropriate support as it progresses.


![Is Dementia Inherited? [Know the Facts] Is dementia Inherited discussed](https://readementia.com/wp-content/uploads/2024/02/Is-dementia-Inherited-discussed-720x300.jpg)


 Is dementia inherited with
Is dementia inherited with  Huntington’s disease
Huntington’s disease Presently more than 20 alterations in the DNA sequence in the gene have been reported. The characteristics of the disease correlate with the different mutation types.
Presently more than 20 alterations in the DNA sequence in the gene have been reported. The characteristics of the disease correlate with the different mutation types.